Celiac.com 12/16/2011 - To date, symptoms of gastroesophageal reflux disease (GERD) - heartburn and acid regurgitation - have been among the only GI symptoms absent from the list of common manifestations of celiac disease. They are usually definitive indicators of gastric acid reflux. But a report from Julio César Bai's group in Buenos Aires notes that at the time of diagnosis, patients with celiac disease were more likely to complain of GERD symptoms than healthy controls. Moreover, maintaining a gluten free diet alleviated these symptoms.  Their results are reported in Clinical Gastroenterology and Hepatology.GERD is a chronic condition usually resulting from the reflux of acidic stomach contents up into the esophagus. It is commonly treated with proton pump inhibitors, but some cases are refractory to this treatment. There has been conflicting data as to whether GERD symptoms are more common in people with celiac, and whether a gluten free diet might help. Dr. Bai's group designed a two pronged study to answer these questions: They undertook a cross sectional analysis of 133 people upon their diagnosis with celiac over the course of 2005, and a longitudinal assessment of 53 of them as they maintained a gluten free diet over the next four years.
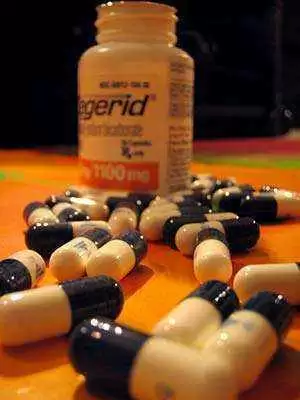
Their results are reported in Clinical Gastroenterology and Hepatology.GERD is a chronic condition usually resulting from the reflux of acidic stomach contents up into the esophagus. It is commonly treated with proton pump inhibitors, but some cases are refractory to this treatment. There has been conflicting data as to whether GERD symptoms are more common in people with celiac, and whether a gluten free diet might help. Dr. Bai's group designed a two pronged study to answer these questions: They undertook a cross sectional analysis of 133 people upon their diagnosis with celiac over the course of 2005, and a longitudinal assessment of 53 of them as they maintained a gluten free diet over the next four years.
At the time of their diagnosis, the proportion of celiac with reflux was six-fold higher than that in the the 70 healthy controls included in the study. Interestingly, more severe reflux symptoms were associated with the classical, rather than the silent, presentation of celiac disease. However, it should be noted that this was somewhat of a selected population; these data were obtained from patients coming to a malabsorption clinic, where the classic presentation of celiac is more prevalent than the silent type. Moreover, for whatever reason, these healthy volunteers had less GERD symptoms than is usually reported. After three months on a gluten free diet symptoms were comparable to those seen in healthy controls. Interestingly, though, this was the case for patients who reported only partially complying to a gluten free diet as well as those who adhered to it strictly.
Celiac.com Sponsor (A12):
Because these symptoms are alleviated upon assumption of a gluten free diet, the authors hypothesize that they might be caused by a nontraditional mechanism in celiac patients rather than by actual reflux. One suggestion they posit is reduced upper gastrointestinal motility, and another is a permeability defect in the stratified esophageal epithelium. In an editorial accompanying the paper, delayed gastric emptying and disturbed neuroendocrine control of upper GI function are floated potentially contributing to GERD symptoms in untreated celiac. Further research would have to be done to bear out these and other ideas.
Nachman F, Vázquez H, González A, Andrenacci P, Compagni L, Reyes H, Sugai E, Moreno ML, Smecuol E, Hwang HJ, Sánchez IP, Mauriño E, Bai JC. Gastroesophageal reflux symptoms in patients with celiac disease and the effects of a gluten-free diet. Clin Gastroenterol Hepatol. 2011 Mar;9(3):214-9. Epub 2010 Jun 30.
Source:
- Open Original Shared Link





Recommended Comments