Celiac.com 12/30/2024 - Celiac disease is an autoimmune disorder in which the immune system launches an aggressive response against gluten, a protein found in wheat, barley, and rye. This response damages the intestinal lining, leading to debilitating symptoms and requiring lifelong adherence to a strict gluten-free diet. However, groundbreaking research recently published in Gastroenterology unveils new insights into how the immune response to gluten begins, potentially paving the way for innovative therapies—and perhaps even a cure.
Understanding Celiac Disease and the Role of Gluten
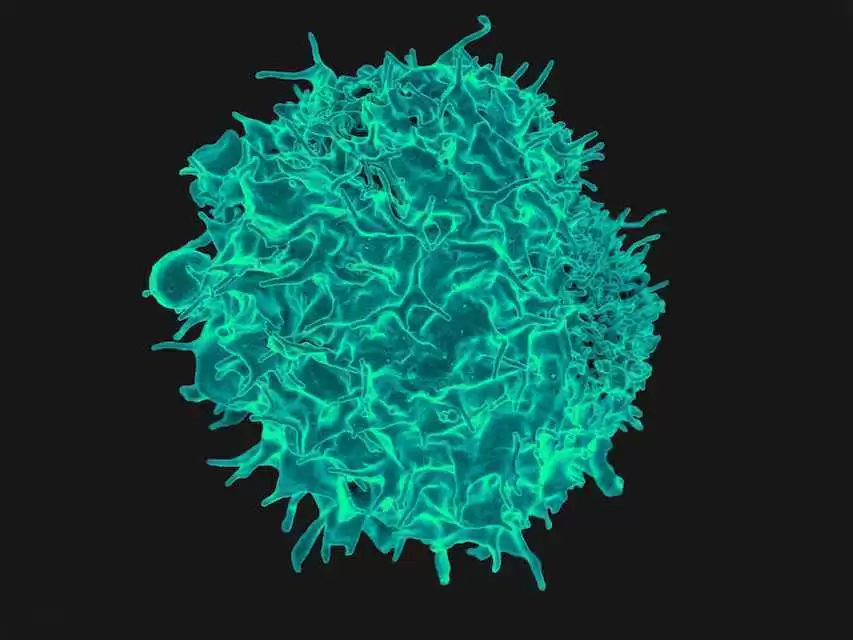
For individuals with celiac disease, consuming gluten triggers an immune response that damages the intestinal epithelial cells (IECs), which line the upper intestine. This damage can cause severe gastrointestinal symptoms, nutrient malabsorption, and a cascade of systemic effects. The key culprit in this immune reaction has long been identified as CD4+ T-cells, specialized immune cells activated when gluten-derived antigens are presented to them by molecules known as MHC class II proteins.
Celiac.com Sponsor (A12):
Until now, researchers believed that antigen-presenting cells, such as dendritic cells and macrophages, were the primary facilitators of this process. However, the new study has identified IECs themselves as crucial players in gluten antigen presentation and subsequent T-cell activation.
The Discovery: Epithelial Cells Take Center Stage
The study demonstrates that intestinal epithelial cells expressing human MHC class II proteins (HLA-DQ2.5) play a pivotal role in activating gluten-specific CD4+ T-cells. This process was observed both in patients with active celiac disease and in a specialized mouse model genetically engineered to express the human MHC class II molecule.
Key findings include:
- Epithelial MHCII Expression: In both human patients with active celiac disease and gluten-immunized mice, intestinal epithelial cells were shown to express MHCII molecules. This expression increased significantly when the cells were exposed to interferon-gamma (IFN-γ), a pro-inflammatory cytokine.
- CD4+ T-Cell Activation: In laboratory co-culture experiments, gluten exposure led to a robust activation of CD4+ T-cells. This activation was marked by increased cell proliferation, upregulation of activation markers, and the release of inflammatory cytokines such as interleukin-2, IFN-γ, and interleukin-15.
- Microbial Influence: The study also revealed that gluten pre-digested by elastase-producing bacteria (Pseudomonas aeruginosa) heightened the activation of CD4+ T-cells. Interestingly, this effect was absent when a mutant strain of the bacteria lacking elastase production was used.
These findings highlight the complexity of the immune response in celiac disease and the previously underestimated role of IECs in driving the process.
Implications for Celiac Disease Treatment
The discovery of epithelial cells’ role in gluten antigen presentation opens new doors for therapeutic strategies. By targeting the mechanisms within IECs that facilitate T-cell activation, researchers could potentially disrupt the immune cascade at its source.
Potential treatment approaches include:
- Inhibiting MHCII Expression: Therapies designed to suppress MHC class II expression in IECs may prevent gluten antigen presentation to CD4+ T-cells.
- Blocking Pro-inflammatory Signals: Drugs targeting IFN-γ or other inflammatory cytokines might reduce MHCII upregulation, minimizing immune activation.
- Modulating Gut Microbiota: Since microbial elastase enhances gluten antigen processing, altering the gut microbiome composition could mitigate its impact on immune activation.
While these strategies are still in the early stages of exploration, they represent a significant step toward disease-modifying treatments for celiac disease.
A Step Closer to a Cure
Currently, the only treatment for celiac disease is a strict, lifelong gluten-free diet. This diet is challenging to maintain and does not completely eliminate the risk of inadvertent gluten exposure, which can trigger severe symptoms. The study’s findings offer hope for a future where treatments go beyond symptom management to address the underlying cause of the disease.
By pinpointing the initial stages of the immune response to gluten, researchers have provided a blueprint for interventions that could potentially prevent or reverse the condition. While a cure remains on the horizon, the knowledge gained from this research brings it closer to reality.
A New Era in Celiac Disease Research
This groundbreaking study sheds light on the critical role of intestinal epithelial cells in celiac disease pathogenesis, reshaping our understanding of how gluten triggers the immune response. The findings not only deepen scientific insight but also offer practical pathways for developing innovative treatments.
For the millions of people living with celiac disease, this research represents a beacon of hope—an indication that one day, the burden of a gluten-free life may be replaced with the freedom to enjoy food without fear. As researchers continue to build on these findings, the dream of a cure for celiac disease feels more attainable than ever.
Read more at: gastrojournal.org






Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now