
Celiac.com 02/05/2023 - If you have celiac disease symptoms, for example chronic diarrhea, anemia, bloating, abdominal pain, rashes, are in a higher risk group, etc., your doctor may order a blood test for celiac disease. Note that before doing any blood tests for celiac disease you must be eating gluten for a while beforehand, and the amount and length of time can vary, but is somewhere between 2 slices of wheat bread daily for 6-8 weeks and 1/2 slice of wheat bread or 1 wheat cracker for 12 weeks, otherwise you may end up with false negative results.
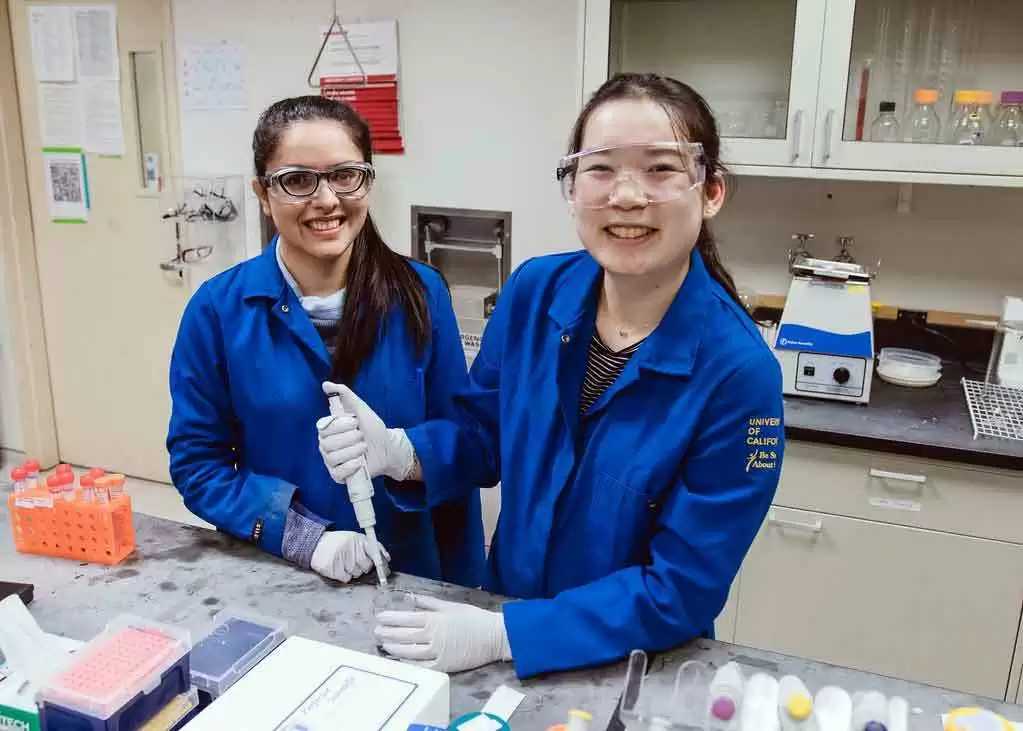
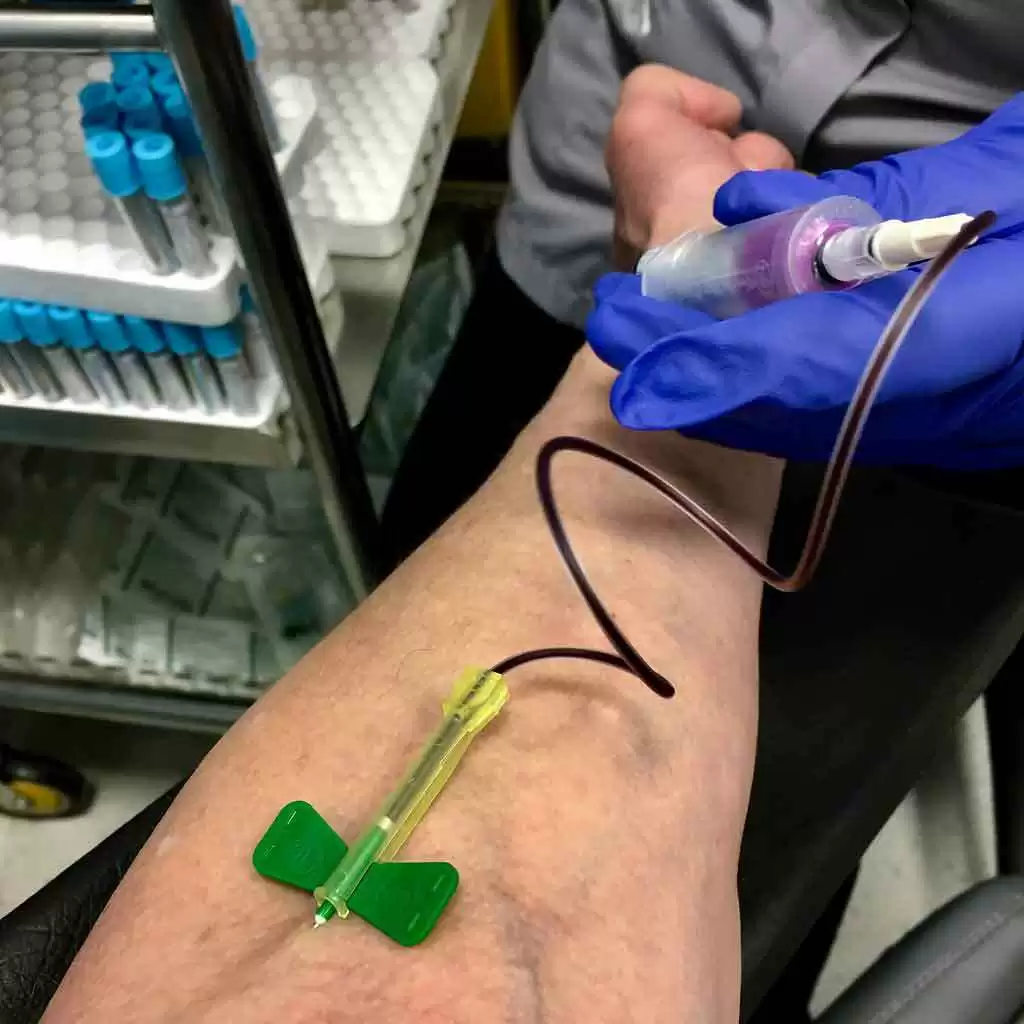
For a celiac disease antibody test, a clinician collects a small amount of the patient's blood. The sample is then sent to a lab, where the blood cells are then removed, and the test is conducted.
Celiac Disease Blood Tests
Celiac.com Sponsor (A12):
Note that the accuracy and specificity of each test can vary depending on the laboratory performing the test, the specific method used, and the population being tested. Sensitivity refers to the ability of a test to correctly identify individuals with the condition (true positive rate), while specificity refers to the ability of a test to correctly identify individuals without the condition (true negative rate).
tTG-IgA (tissue transglutaminase IgA) Blood Test for Celiac Disease
This test measures the levels of IgA antibodies to tissue transglutaminase, an enzyme that is involved in the immune response to gluten in those who have celiac disease.
The test is estimated to have a sensitivity of approximately 90%, which means that it correctly identifies 90% of people with celiac disease. It also has a high specificity of around 95%, which means that it correctly identifies 95% of people who do not have celiac disease.
Other Names for the tTG-IgA Test:
- Tissue Transglutaminase IgA Test
- Anti-Tissue Transglutaminase IgA Test
- tTG-IgA Blood Test
- tTG-IgA Serology Test
- IgA-tTG Antibody Test
- Tissue Transglutaminase Antibody IgA Assay
tTG-IgG (tissue transglutaminase IgG) Blood Test for Celiac Disease
This test measures the levels of antibodies to tissue transglutaminase, but it specifically measures IgG antibodies rather than IgA antibodies which are produced in people who eat gluten and have celiac disease. It is not as sensitive or specific as the tTG-IgA test, but it may be useful in cases where a person has an IgA deficiency, which can occur in approximately 2-3% of people with celiac disease. In these cases, the tTG-IgG test may be positive while the tTG-IgA test is negative. However, the tTG-IgG test is not recommended as a first-line screening test for celiac disease.
The sensitivity of the tTG-IgG blood test is generally high, ranging from 85% to 98%. This means that the test can accurately detect celiac disease in a significant percentage of people who have the condition.
The specificity of the tTG-IgG blood test is also high, typically around 90% to 98%. This indicates that the test can effectively rule out celiac disease in individuals who do not have the condition.
Other Names for the tTG-IgG Test:
- Tissue Transglutaminase IgG Test
- Anti-Tissue Transglutaminase IgG Test
- tTG-IgG Blood Test
- tTG-IgG Serology Test
- IgG-tTG Antibody Test
- Tissue Transglutaminase Antibody IgG Assay
EMA-IgA (endomysial antibodies IgA) Blood Test for Celiac Disease
This is a highly accurate test for celiac disease, that requires specialized expertise to perform and interpret, and it is more expensive than other blood tests. It is generally used as a last test to confirm celiac disease after a positive tTG-IgA test.
The sensitivity of a test refers to its ability to correctly identify individuals with the condition. For the EMA-IgA blood test, the sensitivity is generally very high, ranging from 90% to 98%. This means that the test can accurately detect celiac disease in a significant percentage of people who have the condition.
The specificity of a test refers to its ability to correctly identify individuals without the condition. For the EMA-IgA blood test, the specificity is also high, typically around 95% to 100%. This indicates that the test can effectively rule out celiac disease in individuals who do not have the condition.
Other Names for the EMA-IgA Test:
- Endomysial Antibodies IgA Test
- Anti-Endomysium Antibodies IgA Test
- Endomysial Antibody IgA Assay
- EMA IgA Blood Test
- EMA-IgA Serology Test
- Endomysium IgA Ab
DGP-IgA and DGP-IgG (Deamidated Gliadin Peptide) Blood Tests for Celiac Disease
These tests measure the levels of antibodies in the blood, but specifically targets deamidated gliadin peptides, which are a type of gluten protein that can trigger an immune response in people with celiac disease. The tests are not always included in adults, but should be in cases with IgA deficiency. The tests should always be included when screening children, especially if they are under 2 years old. The DGP tests were created to detect celiac disease in those with IgA deficiency, and there are here is more information about them:
- DGP-IgA Test: This test measures the levels of IgA antibodies specific to deamidated gliadin peptide. IgA antibodies are produced by the immune system in response to gluten exposure. In individuals with celiac disease who produce normal levels of IgA, a positive DGP-IgA test result suggests the presence of ongoing immune response to gluten.
- DGP-IgG Test: The DGP-IgG test measures IgG antibodies against deamidated gliadin peptide. IgG antibodies are another type of immune response and may be elevated in individuals with celiac disease who have IgA deficiency (a common occurrence in celiac disease).
The DGP-IgA test is considered to have high sensitivity and specificity. In general, the DGP-IgA test has been reported to have a sensitivity ranging from 75% to 95% and a specificity ranging from 90% to 100%. Overall, the DGP tests, including DGP-IgA and DGP-IgG, exhibit a sensitivity of approximately 85-95% and a specificity of about 95-98%.
Other Names for the DGP-IgA Test:
- Gliadin Peptide Antibody IgG (Immunoglobulin A)
- Anti-Gliadin Antibody IgA (AGA IgA)
- Anti-Gliadin IgA Antibody (AGA IgA)
- Anti-Gliadin IgA (AGA IgA)
- Anti-Gliadin Immunoglobulin A Antibody (AGA IgA)
- Anti-Deamidated Gliadin Peptide IgA (DGP IgA)
- Anti-Deamidated Gliadin Antibody IgA (DGP IgA)
The sensitivity of the DGP-IgG test is reported to range from 75% to 85%, which means it can correctly identify individuals with the condition in about 75% to 85% of cases. The specificity of the DGP-IgG test is reported to range from 75% to 95%, which means it can correctly identify individuals without the condition in about 75% to 95% of cases. Overall, the DGP tests, including DGP-IgA and DGP-IgG, exhibit a sensitivity of approximately 85-95% and a specificity of about 95-98%.
Other Names for the DGP-IgG Test:
- Gliadin Peptide Antibody IgG (Immunoglobulin G)
- Anti-Gliadin Antibody IgG (AGA IgG)
- Anti-Gliadin IgG Antibody (AGA IgG)
- Anti-Gliadin IgG (AGA IgG)
- Anti-Gliadin Immunoglobulin G Antibody (AGA IgG)
- Anti-Deamidated Gliadin Peptide IgG (DGP IgG)
- Anti-Deamidated Gliadin Antibody IgG (DGP IgG)
IgA Levels/Deficiency Blood Test
This should always be included in any blood panel for celiac disease, but it does not test directly for celiac disease, and is done to determine the accuracy of the other blood tests. People who are IgA deficient may score lower, of have no measurable levels on certain celiac disease blood tests. This test measures the levels of Immunoglobulin A (IgA) in the bloodstream. IgA is an important antibody that plays a significant role in the immune system, particularly in protecting the body's mucosal surfaces (e.g., respiratory and digestive tracts). Low IgA levels can indicate IgA deficiency, a condition where the body does not produce enough IgA, leading to an increased risk of infections and other health issues. The IgA Levels/Deficiency Test helps healthcare providers diagnose and monitor IgA-related conditions.
Other Names for the IgA Levels/Deficiency Test:
- Immunoglobulin A (IgA) Test
- Total IgA Test
- Serum IgA Test
- IgA Serum Levels Test
- IgA Blood Test
- IgA Quantitative Test
- IgA Antibody Test
- IgA Immunodeficiency Test
Celiac Disease Blood Antibody Screening is ~98% Accurate in Adults Using the Mayo Clinic Protocol
A celiac disease blood panel includes several tests to determine whether someone has celiac disease. These tests are very specific because certain antibodies only appear in those with gluten sensitivity, celiac disease and/or dermatitis herpetiformis.
Testing begins with a test called Immunoglobulin A (IgA). If the results are normal, then a Tissue transglutaminase, antibody, IgA test is given. A weak positive should lead to the following tests:
- Endomysial antibodies (IgA) and;
- Gliadin (deamidated) antibody, IgA.
If the initial Immunoglobulin A (IgA) test is lower than normal, then these two tests should be done:
- Tissue transglutaminase antibodies, IgA and IgG profle.
- Gliadin (deamidated) antibodies evaluation, IgG and IgA.
If the initial Immunoglobulin A (IgA) test is below the level of detection (<1.0 mg/dL), then these two tests should be done:
- Tissue transglutaminase (tTG) antibody, IgG.
- Gliadin (deamidated) antibody, IgG.
It sounds complicated, but it's pretty standard procedure now, and when blood screening is done this way the results for celiac disease are ~98% accurate.
Many People Can Be Diagnosed Using Only Blood Tests and No Biopsy
According to the latest research, if the blood test results are at certain high levels that range between 5-10 times the reference range for a positive celiac disease diagnosis, it may not be necessary to confirm the results using an endoscopy/biopsy:
- Blood Test Alone Can Diagnose Celiac Disease in Most Children and Adults
- TGA-IgA at or Above Five Times Normal Limit in Kids Indicates Celiac Disease in Nearly All Cases
- No More Biopsies to Diagnose Celiac Disease in Children!
Biopsy Still Standard in Adult Celiac Diagnosis
After positive blood tests some doctors still require a biopsy to confirm the diagnosis. However, this is changing, as new techniques allow doctors to accurately detect celiac disease in adults without a biopsy.
Remember, nearly all tests and screening for celiac disease require the patient to be eating a gluten-containing diet before testing, usually you should be eating at least 1/2 slice of wheat bread or 1 wheat cracker daily for at least 2 weeks before the endoscopy. Be sure to check with your doctor for the latest protocol.
Blood Tests for Follow Up Care
Blood tests may also be useful in follow up care in those with celiac disease to confirm that their diet is indeed free of gluten. Also, because of the lack of standardization, keep in mind that blood test results may not be directly comparable from one lab to the next.
More Celiac Disease Testing Resources
- What is a Gluten Challenge and How Long Must it Last?
- Interpretation of Celiac Disease Blood Test Results
- Ten Facts About Celiac Disease Genetic Testing
Blood Test Questions on the Celiac Disease and Gluten-Free Forum
Read more at mayocliniclabs.com









Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now