Celiac.com 06/29/2010 - Properly diagnosing children with celiac disease in conditions where there may be environmental or other causes for classic celiac-associated symptoms, such as malnutrition, diarrhea, and failure to thrive, can present challenges to clinicians.
A clinical team conducted an assessment of celiac disease blood screens in symptomatic 12 to 36 month-old children. The research team included Inês Cristina Modelli; Lenora Gandolfi; Rodrigo Coutinho de Almeida; Gloria Maria A. C. Araújo; Marilúcia de Almeida Picanço; and Riccardo Pratesi.
Celiac.com Sponsor (A12):
They are associated with the Graduate Program in Health Sciences at the University of Brasilia School of Health Sciences, the Pediatric Department at the Brasilia University Hospital, and the Pediatric Research Center and Celiac Disease Investigation Center at the University of Brasilia School of Medicine in Brazil.
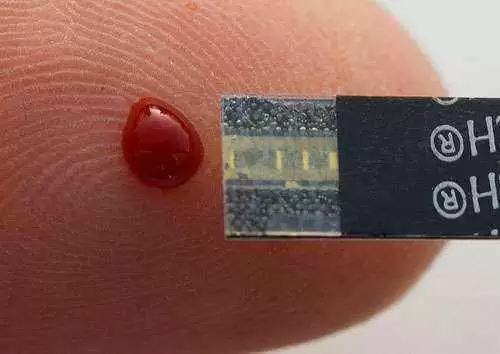
The clinicians wanted to assess rates of celiac disease in a group of 12 to 36 month-old children using immunoglobulin antibodies against gliadin (IgG and IgA-AGA), against endomysium (IgA-EMA), and anti-human tissue transglutaminase (IgA-tTG) screens.
For the study, the team enrolled 114 boys and 100 girls, aged 12 to 36 months, all following a gluten-containing diet. The team performed IgG and IgA-AGA, IgA-tTG and IgA-EMA blood tests for each patient. The team took biopsies from all children who showed one or more positive blood test, except those for whom IgG-AGA was the only positive result.
In cases where IgG-AGA was the only positive result, the team used polymerase chain reaction (PCR) HLA genotyping to identify the celiac disease predisposing alleles. HLA genotyping also allowed the team to confirm diagnosis in children flagged as celiac by means of positive serologic testing and compatible biopsy results.
The team found that 131 kids showed normal results. PCR showed the presence of celiac disease predisposing alleles in ten out of 68 children who tested positive on just the IgG-AGA test. Four kids had positive results on all four blood tests, while a fifth child showed positive results IgG and IgA-AGA and IgA-tTG, but showed negative results for IgA-EMA. All five children submitted to jejunal biopsies, which showed classic celiac lesions.
Symptomatic children from 12- to 36-months old that had not been previously diagnosed with celiac disease showed celiac prevalence of 2.3%.
This study shows several things. First, the data reflect the challenges of diagnosing celiac disease in areas where environmental or other causes for classic celiac-associated symptoms might interfere with proper diagnosis. The results also show the advantages of considering biopsies in cases of conflicting or incomplete blood screens in symptomatic children who may be subject to environmental and other mitigating factors.
That such symptomatic children show celiac disease rates that are more than double the general population shows that clinicians attempting diagnosis under such circumstances should be both diligent and exhaustive in their efforts. As it is, symptomatic children with celiac disease are going undiagnosed. To properly diagnose such cases, clinicians should consider any environmental or other causes for classic celiac-associated symptoms that might interfere with proper diagnosis.
There is no reason to assume that these results are exclusive to Brazil. There's no reason to assume these results wouldn't apply anyplace where environmental and other causes might interfere with diagnosis of celiac disease in symptomatic children, including regions of rural and urban poverty.
Source:
- Open Original Shared Link






Recommended Comments
There are no comments to display.