Celiac.com 10/07/2013 - People with non-celiac gluten-sensitivity often report gut and non-gut symptoms shortly after eating gluten; symptoms disappear on gluten-free diets, although these patients have no serologic markers of celiac disease, and no intestinal damage. However, there is no evidence to suggest any changes to blood or mucosa in those individuals.
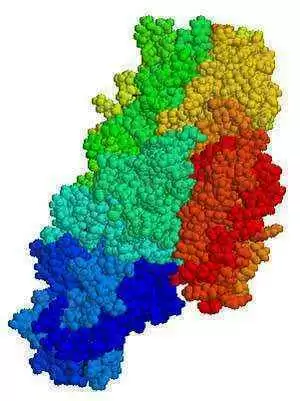 To better understand non-celiac gluten sensitivity, a research team recently assessed immunologic responses of duodenal mucosa samples and peripheral blood basophils, isolated from NCGS patients, after exposure to gliadin.
To better understand non-celiac gluten sensitivity, a research team recently assessed immunologic responses of duodenal mucosa samples and peripheral blood basophils, isolated from NCGS patients, after exposure to gliadin.
Celiac.com Sponsor (A12):
The research team included Cristina Bucci, Fabiana Zingone, Ilaria Russo, Ivonne Morra, Raffaella Tortora, Norberto Pogna, Giulia Scalia, Paola Iovino, and Carolina Ciacci. They are affiliated with CEINGE in Naples, Italy; the Consiglio per la Ricerca e la Sperimentazione in Agricoltura in Rome, Italy; the Gastrointestinal Unit of the Department of Medicine and Surgery at the University of Salerno in Salerno, Italy; and with the Gastrointestinal Unit at the Department of Clinical and Experimental Medicine of Federico II University of Naples.
Between January 2010 and July 2011, the research team gathered mucosa samples from 34 celiac disease patients who followed gluten-free diets for at least 6 months, 35 patients with untreated celiac disease, 16 patients with non-celiac gluten sensitivity (NCGS) and 34 healthy control subjects. The team diagnosed non-celiac gluten sensitivity based on patient symptoms and current diagnositic guidelines.
For each of the 119 patients, the team conducted a complete clinical evaluation to exclude celiac disease while on a gluten-containing diet, a skin prick test to exclude wheat allergy, and upper endoscopy at 2 tertiary medical centers in Italy.
After incubating each biopsy sample with gliadin, the team measured inflammatory markers, including anti-phosphotyrosine-monoclonal antibody (PY99), HLA-DR, intercellular cell adhesion molecule-1 (ICAM-1), CD3, CD25 and CD69.
After incubation with gliadin, mucosa samples from the 69 patients with celiac disease showed increased immunofluorescence intensity for early and delayed markers of inflammation. They also found low levels of some of these markers in three patients with non-celiac gluten sensitivity and three controls.
The team found normal mucosal architecture in 56.3% of patients with non-celiac gluten sensitivity. The remaining seven patients showed increased intraepithelial infiltration, but without eosinophils.
They found no villous atrophy in patients with non-celiac gluten sensitivity, and no significant increases in the levels of CD63 and CD203c.
The team did find that one patient each in the NCGS and control groups, whose results indicated only weak PY99 and ICAM-1 positivity, also had Helicobacter pylori infection.
Unlike mucosa from patients with celiac disease, once incubated with gliadin, mucosa from patients with NCGS does not express markers of inflammation, nor does the gliadin activate their basophils. The in vitro gliadin challenge therefore should not be used to diagnose NCGS.
This study does suggest that wheat components, other than proteins, might be associated with GI symptoms in patients with IBS, and should be assessed for a possible role in the pathogenesis of NCGS.
Source:
- Open Original Shared Link





Recommended Comments
There are no comments to display.