
Celiac.com 06/19/2020 (Revised 06/24/2020) - It is not uncommon to have received blood testing from your doctor to see if you have celiac disease, and it comes back negative, when in fact your body is actually having a problem and you are on the celiac spectrum. The tests most doctors use to determine whether or not someone has celiac disease are very accurate for end stage celiac disease-after you have total villous atrophy, but not earlier stages of the disease (1). In those earlier situations, these tests often come back negative, even though you truly have a problem and are reacting to wheat moving towards total villous atrophy (1, 2, 3, 4, 5). It’s the wrong test.
If you have an earlier stage in terms of the amount of damage incurred, the standard blood tests can be wrong over 70% of the time giving false negatives
Standard blood tests for celiac disease have been extremely accurate and dependable if a person has total villous atrophy celiac disease. However, the accuracy of the blood test results for the two accepted blood markers (Endomysium and Tissue Transglutaminase) with anything less than total villous atrophy drops tremendously (to as low as being wrong 7 out of 10 times) (8,9). The reason these tests are often wrong in some people is that the research to validate the test used subjects who all had been diagnosed with celiac disease which by definition was total villous atrophy (Marsh IIIa,b,c). The earlier stages, Marsh 1 and 2 by most are considered ‘potential celiac disease’. So, when researchers were looking to validate if their blood tests were accurate in diagnosing celiac disease, they tested the blood of people diagnosed with celiac disease (total villous atrophy). And in that scenario, endomysium and tissue transglutaminase are highly accurate.
Celiac.com Sponsor (A12):
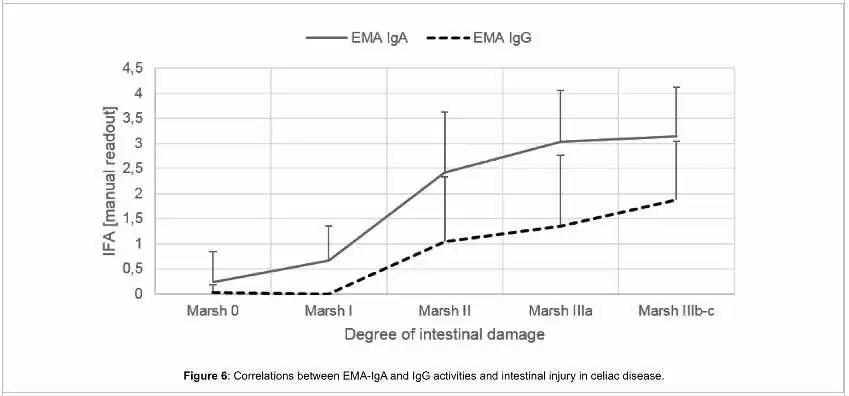
from Lerner A, Jeremias P, Neidhöfer S, Matthias T (2017) Comparison of the Reliability of 17 Celiac Disease Associated Bio-Markers to Reflect Intestinal Damage. J Clin Cell Immunol 8: 486.
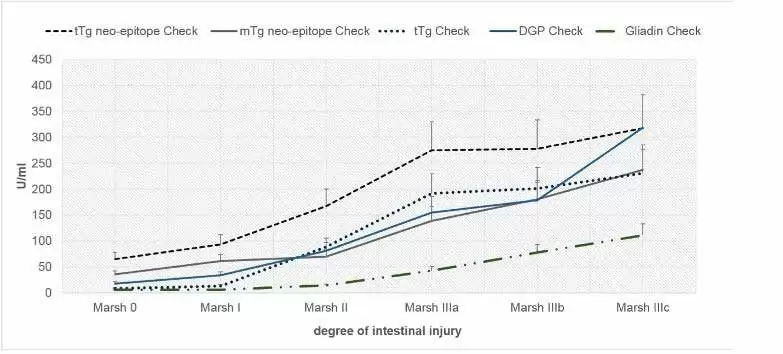
from Lerner A, Jeremias P, Neidhöfer S, Matthias T (2017) Comparison of the Reliability of 17 Celiac Disease Associated Bio-Markers to Reflect Intestinal Damage. J Clin Cell Immunol 8: 486.
Why? Celiac disease is defined as total villous atrophy. However, you don’t just magically go to sleep one night fine and wake up the next morning with total villous atrophy celiac disease. This disease, like all diseases, needs to be looked at more as a spectrum. That’s why Prof. Michael Marsh identified the spectrum of celiac disease development (Marsh I, II, III a, b, c). Bottom line? The test for total villous atrophy celiac disease (Marsh III a, b, c) are not the tests to rely on for earlier phases of the spectrum (Marsh I, II).
The end result is many people have been told they do not have celiac disease and wheat is not a problem continue eating this food that is leading them further down the path of autoimmune disease. And of course, the tests for celiac disease are NOT the tests for the spectrum of Wheat Related Disorders (9).
Predictive autoimmunity can tell you what areas of your body are under attack. Identifying an autoimmune mechanism early in the spectrum of development gives an opportunity to address it before there is so much tissue damage, now you have an autoimmune disease. Autoimmunity is the number 3 cause of death and highly preventable. If you could peek inside and determine what is going on before it does irreparable damage, it gives you a window of opportunity to address the problem early on and change the course of your health. This is called Predictive Autoimmunity (30). Identifying that you are on the celiac spectrum at Marsh I, gives you the opportunity to take action (gluten-free diet) and prevent progressing to Marsh III total villous atrophy. So the tests that are highly accurate for Marsh III are the wrong tests for Marsh I and II. They may be helpful and they may be misleading
Gluten, Autoimmunity, and Your Gut
Dr. Alessio Fasano is the chair of pediatric gastroenterology at Mass. General Hospital, Harvard, and director of Mucosal Immunology and Biology Research Center at Mass General Hospital for Children. He has done extensive research in the area of mucosal lining of the gut. He discovered, in the early 2000’s, a trilogy present in the development of autoimmunity: genetics, triggers, and intestinal permeability. (10) With celiac, we all know this – DQ2/DQ8, gluten, leaky gut = vulnerability to developing celiac disease.
In the last 15 years, research has continued to expand to include two more features - thus a total of 5 components in the development of autoimmune diseases. In addition to genetics, environmental triggers and intestinal permeability, we now know that a dysbiotic microbiome and a systemic inflammatory immune response are involved. (11)
This is important in our understanding of treatment. You can arrest the development of autoimmunity by healing the gut and addressing intestinal permeability. The majority of people with leaky gut do not show symptoms in the gut. A leaky gut spews out macromolecules into the blood stream that travel throughout your body that are considered foreign objects that your immune system will protect you from. And the resulting systemic inflammation from a leaky gut can affect any area of your body. And what are the most common triggers that will trigger a leaky gut? Gluten and small intestinalal bacteria overload. (11)
Dangers of a Gluten-Free Diet
Now this is a ‘Big Picture’ concept, but when you read the science it is clear that no one can fully digest the proteins in wheat (11, 12, 13, 14). It is indigestible to all humans, and in every single person causes a transient state of intestinal permeability (12, 13). Having said that, not everything about wheat is bad. Wheat (78%) and barley (3%) account for 78 - 81% of total prebiotics in the Western diet (14, 15, 16). When you remove wheat from your diet, a large percentage of the good bacteria will likely starve. This may be a contributing factor to the jaw-dropping statistic from the largest study ever done on mortality and celiac disease, that being diagnosed with celiac disease is associated with an 86% increased risk of mortality from a cardiovascular incident within 1 year (18). Just by being diagnosed. As far as I know, no one has pursued further research on this fact. What is different after diagnosis? People go on a gluten-free diet. What else? For most people, nothing else-they just stat eating gluten-free foods. You MUST be conscious of replacing the loss of prebiotics in your diet. Replacing wheat-based products with gluten-free products is a landmine. The vast majority of gluten-free products do not have prebiotic fibre, are not enriched, and are just tasty white paste. There’s nothing wrong with a gluten-free blueberry muffin once in a while, or gluten-free pasta on occasion. But these products are not healthy for you and can NOT be the cornerstone of your new diet. Be mindful of this at the onset of starting your gluten-free diet, so that you replenish your body with the necessary prebiotic nutrients your microbiome needs to increase diversity and balance. (14)
So many people make the same newbie mistakes of just shopping in the gluten-free aisle and walk away with gluten-free cookies and snacks. I’m sorry to say that those are pretty much just as unhealthy, or worse, than the gluten versions. They just lack the antigen gluten.
You need to look towards the produce aisle, vary your food choices from day to day, eat a wide variety in colour and types of organic fruits and vegetables, eat fermented foods rich in probiotics, and feed that good bacteria in your gut with foods that are prebiotics (root vegetables daily).
I highly recommend finding a Certified Gluten-free Practitioner (CGP) who has received extensive training in celiac disease, gluten sensitivities, wheat-related disorders and autoimmunity. That is the most comprehensive training out there in this area. Find a CGP in your area-they’re all over the world, and most do on-line private consults.
Addressing the intestinal permeability that has been developing with every exposure to wheat (12), within 5 minutes of wheat coming out of the stomach into the small intestine (20), is a game-changer in your overall health. There are over 300 autoimmune conditions. With the ‘Gateway’ in the development of autoimmune diseases being intestinal permeability, addressing this, and focusing on healing the gut can bring big rewards.
Heal the Gut
- Identify and eliminate your triggers.
- Reduce inflammation.
- Reduce stress.
The following supplements all have many studies showing their value in addressing intestinal permeability: Glutamine (21), Fish oils (22), Vitamin D (23), Colostrum (24), Turmeric (25), Pre (26) and Probiotics (27). Each of these basic nutrients modulates (has their hands on the steering wheel) of genes to reduce inflammation achieving a similar end goal, but they each work in different ways. Using a pleiotropic approach ensures success (great scrabble word-pleiotropic-means ‘all roads lead to Rome’.
When you have a gluten-related disorder, the treatment is a strict gluten-free diet - without exception. Don’t let the treatment be the trigger for more problems. I’m known for the saying “You can’t be a little pregnant, you can’t have a little gluten” (if your immune system is activated fighting any of the peptides of wheat). Cheating once-per-month increases your risk of early death 6-fold! (19)
Take measures to protect yourself against nutritional and vitamin deficiencies associated with a gluten-free diet. The benefits of a ‘Coach’ to learn the correct basics through this transition cannot be overemphasized (28, 29). A CGP, Nutritionist, trained Registered Dietician, Health Coach, … are invaluable in you learning the basics of this transition into a new way of eating. Eat different colors of the rainbow at every meal, every day. It will help restore balance to your gut health and rebalance your immune system.
If you’re going to do this alone, avoid wheat (gluten), dairy, and added sugar for a month. Eat nutrient dense organic foods, such as quinoa, amaranth, vegetables, and quality meats. Gauge how you feel. Is your weight better managed? Do your hands and feet no longer feel cold? Are you able to think more clearly? If so, continue to eliminate those offending foods and eat a varied diet rich in nutrients. If you reintroduce and notice a problem, now you know those were foods that are inflammatory to you. And be careful of your tricky mind. Humans are the only species on the planet that finds something that works, and they stop doing it!
References:
- Lerner A, Jeremias P, Neidhöfer S, Matthias T (2017) Comparison of the Reliability of 17 Celiac Disease Associated Bio-Markers to Reflect Intestinal Damage. J Clin Cell Immunol 8: 486
- Immunoglobulin A autoantibodies against transglutaminase 2 in the small intestinal mucosa predict forthcoming coeliac disease.
- Salmi TT, Collin P, Järvinen O, Haimila K, Partanen J, Laurila K, Korponay-Szabo IR, Huhtala H, Reunala T, Mäki M, Kaukinen K.Aliment Pharmacol Ther. 2006 Aug 1;24(3):541-52
- Lack of correlation of degree of villous atrophy with severity of clinical presentation of coeliac disease. Brar P, Kwon GY, Egbuna II, Holleran S, Ramakrishnan R, Bhagat G, Green PH.Dig Liver Dis. 2007 Jan;39(1):26-9
- Seronegative celiac disease: increased prevalence with lesser degrees of villous atrophy. Abrams JA, Diamond B, Rotterdam H, Green PH.Dig Dis Sci. 2004 Apr;49(4):546-50
- Utility in clinical practice of immunoglobulin a anti-tissue transglutaminase antibody for the diagnosis of celiac disease. Abrams JA, Brar P, Diamond B, Rotterdam H, Green PH.Clin Gastroenterol Hepatol. 2006 Jun;4(6):726-30
- Tests for Serum Transglutaminase and Endomysial Antibodies Do Not Detect Most Patients With Celiac Disease and Persistent Villous Atrophy on Gluten-free Diets: a Meta-analysis. Silvester JA, Kurada S, Szwajcer A, Kelly CP, Leffler DA, Duerksen DR.Gastroenterology. 2017 Sep;153(3):689-701
- Screening for celiac disease.Lebwohl B, Green PH.N Engl J Med. 2003 Oct 23;349 (17):1673-4
- Joint BAPEN and British Society of Gastroenterology Symposium on 'Coeliac disease: basics and controversies'. Coeliac disease in the twenty-first century. Dickey W. Proc Nutr Soc. 2009 Aug;68(3):234-41.
- Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Fasano A, Shea-Donohue T. Nat Clin Pract Gastroenterol Hepatol. 2005 Sep;2(9):416-22.
- Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Res. 2020;9:F1000 Faculty Rev-69. Published 2020 Jan 31. doi:10.12688/f1000research.20510.1.
- Celiac Disease and Nonceliac Gluten Sensitivity: A Review. Leonard MM, Sapone A, Catassi C, Fasano A. JAMA. 2017 Aug 15;318(7):647-656.
- Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A.Nutrients. 2015 Feb 27;7(3):1565-76.
- Lerner A, O'Bryan T, Matthias T. Navigating the Gluten-Free Boom: The Dark Side of Gluten Free Diet. Front Pediatr. 2019;7:414. Published 2019 Oct 15.
- Effects of a gluten-free diet on gut microbiota and immune function in healthy adult Human subjects - comment by Jackson. Jackson FW. Br J Nutr. 2010 Sep;104(5):773.
- On the presence of Inulin and Oligofructose as natural ingredients in the western diet Jan Van Loo , Paul Coussement , Leen De Leenheer , Hubert Hoebregs & Georges Smits Critical Reviews in Food Science and Nutrition, Volume 35, 1995 - Issue 6.
- Prebiotic effects of wheat arabinoxylan related to the increase in bifidobacteria, Roseburia and Bacteroides/Prevotella in diet-induced obese mice. Neyrinck AM, Possemiers S, Druart C, Van de Wiele T, De Backer F, Cani PD, Larondelle Y, Delzenne NM. PLoS One. 2011;6(6):e20944.
- Small-intestinal histopathology and mortality risk in celiac disease. Ludvigsson JF, Montgomery SM, Ekbom A, Brandt L, Granath F., JAMA. 2009 Sep 16;302(11):1171-8.
- Mortality in patients with coeliac disease and their relatives: a cohort study. Corrao G, Corazza GR, Bagnardi V, Brusco G, Ciacci C, Cottone M, Sategna Guidetti C, Usai P, Cesari P, Pelli MA, Loperfido S, Volta U, Calabró A, Certo M; Club del Tenue Study Group.Lancet. 2001 Aug 4;358(9279):356-61.
- Confocal endomicroscopy shows food-associated changes in the intestinal mucosa of patients with irritable bowel syndrome. Fritscher-Ravens A, Schuppan D, Ellrichmann M, Schoch S, Röcken C, Brasch J, Bethge J, Böttner M, Klose J, Milla. PJ.Gastroenterology. 2014 Nov;147(5):1012-20.
- Glutamine and the regulation of intestinal permeability: from bench to bedside. Achamrah N, Déchelotte P, Coëffier M.Curr Opin Clin Nutr Metab Care. 2017. Jan;20(1):86-91
- Potential of Omega-3 Polyunsaturated Fatty Acids in Managing Chemotherapy- or Radiotherapy-Related Intestinal Microbial Dysbiosis. Zhang Y, Zhang B, Dong L, Chang P.Adv Nutr. 2019 Jan 1;10(1):133-147.
- Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier. Kong J, Zhang Z, Musch MW, Ning G, Sun J, Hart J, Bissonnette M, Li YC.Am J Physiol Gastrointest Liver Physiol. 2008 Jan;294(1):G208-16.
- Peptide Immunotherapy: Colostrum, A Physician's Reference Guide Hardcover, Keech A., AKS Publishing; 1St Edition edition (2009) ISBN-10: 0692002421.
- Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Aggarwal BB, Harikumar KB.Int J Biochem Cell Biol. 2009 Jan;41(1):40-59.
- Modulation of the gut microbiota by nutrients with prebiotic properties: consequences for host health in the context of obesity and metabolic syndrome. Delzenne NM, Neyrinck AM, Cani PD.Microb Cell Fact. 2011 Aug 30;10 Suppl 1(Suppl 1):S10
- Gut Microbiota in Celiac Disease: Is There Any Role for Probiotics? Pecora F, Persico F, Gismondi P, Fornaroli F, Iuliano S, de'Angelis GL, Esposito S.Front Immunol. 2020 May 15;11:957.
- Factors that influence adherence to a gluten-free diet in adults with celiac disease. Leffler DA, Edwards-George J, Dennis M, Schuppan D, Cook F, Franko DL, Blom-Hoffman J, Kelly CP.Dig Dis Sci. 2008 Jun;53(6):1573-81.
- Gluten-free diet: the medical and nutrition management of celiac disease. See J, Murray JA.Nutr Clin Pract. 2006 Feb;21(1):1-15.
- Predicting and preventing autoimmunity, myth or reality? Harel M, Shoenfeld Y.Ann N Y Acad Sci. 2006 Jun;1069:322-45.








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now