Celiac.com 09/04/2021 - I was recently chided by Melissa Jones. She is a reader who wrote to say that I had missed an important element of the topic when I discussed the discovery of zonulin and the therapeutic promise offered by this discovery. Melissa’s complaint was that I should have included a discussion of the connection with lung disease. I agree. After some reflection, I think that there is a good deal more that should be said about this recently discovered protein, including its connection with lung disease. Excessive amounts of zonulin are produced by those who have intestinal diseases. These particularly include celiac disease and type 1 diabetes. Zonulin is a likely factor in autoimmune thyroiditis, systemic lupus erythematosus, Sjogren’s syndrome, scleroderma, and at least sub-groups of multiple sclerosis patients and many rheumatoid arthritis patients. Zonulin may also be a major factor in the development and maintenance of many learning disorders and psychiatric illnesses. Current research has shown that zonulin weakens protective barriers throughout the body, in the intestines, lungs, blood vessels, skin, and perhaps, the brain. Research has also connected increased zonulin production to gluten consumption, but there may be additional factors that can trigger production and the resulting compromise to the various protective barriers this protein regulates. Lung disease is only one facet of this complex issue.
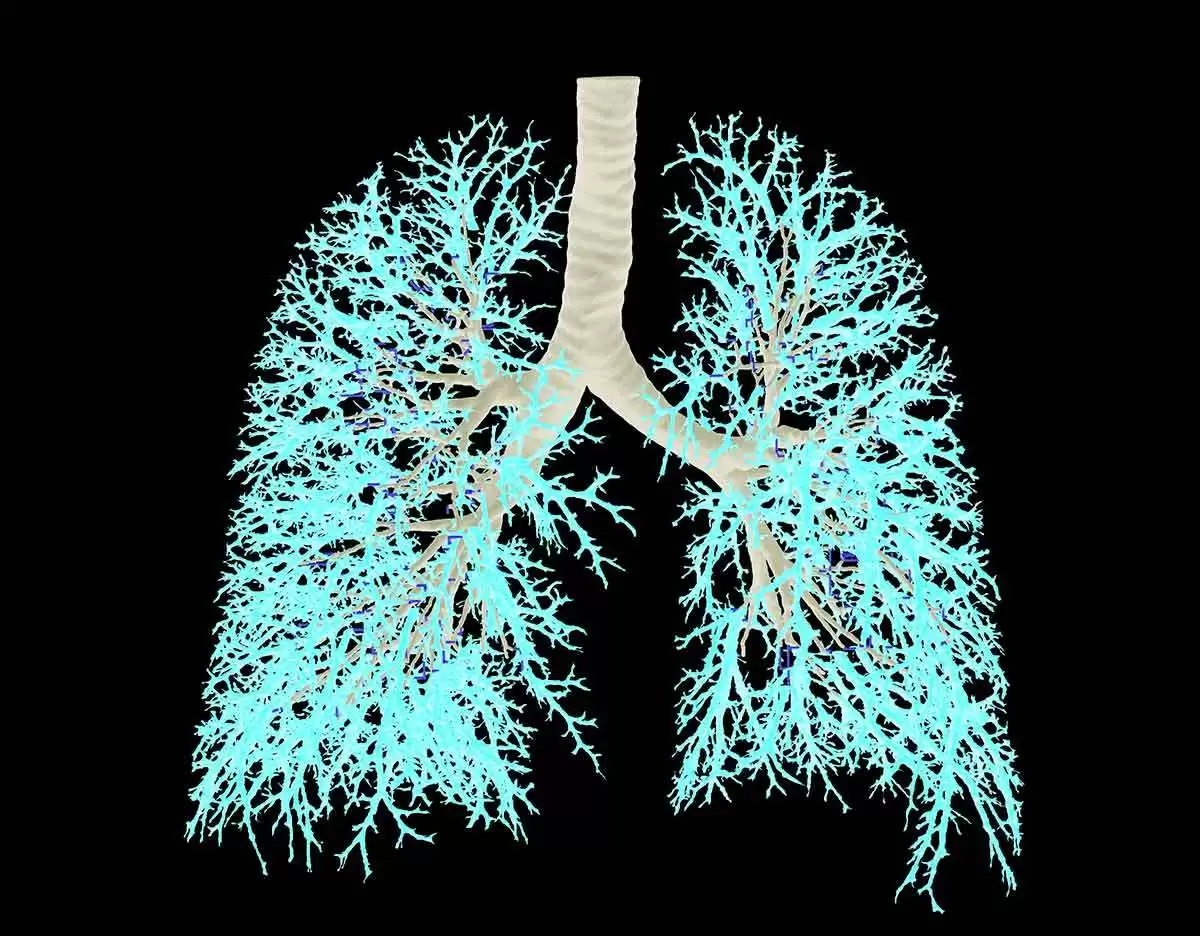
The range and rate of lung diseases among celiac patients is broad and elevated, so Melissa’s concerns are well grounded. Some researchers report a greater frequency of many lung diseases including bird fancier’s lung, farmer’s lung, Idiopathic pulmonary hemosiderosis, lymphocytic bronchoalveolitis, pulmonary sarcoidosis, cavities in the lung walls, fibrosing alveolitis, and while there is some disagreement in the literature, there may also be higher rates and greater severity of asthma among celiac patients. Nonetheless, it should not be surprising that we experience an increased risk of lung disease since there is considerable similarity between the barrier functions of the mucosa of the lungs and that of the intestines. Thus, the search for a drug that can help us maintain the integrity of this barrier could protect against lung disease and provide important benefits for gluten sensitive individuals who are at greater risk of developing breathing problems along with the host of other ailments that involve compromised protective barrier function.
Celiac.com Sponsor (A12):
For instance, investigations of zonulin have the potential to help people with autoimmune diseases. This research may even offer a new, proactive therapy for workers in the baking and milling industries, for severe burn victims who will predictably develop intestinal distress, and for cancer patients who are undergoing radiation treatments. Even patients with skin diseases may be helped. The therapeutic promise of the gluten-free diet for improving various psychiatric diseases, learning disabilities, and behavior problems might also be realized, at long last. The potential therapeutic implications of zonulin research, for a wide range of patients, are startlingly broad.
I attended Blake Patterson’s presentation at the 12th International Celiac Disease Symposium on Saturday, November 11th in New York City. Alba Therapeutics, with Blake Patterson at the helm, is currently developing a drug that is aimed at delivering AT-1001 with meals. This substance blocks zonulin action by cloning the receptors which bind to zonulin but do not relax the tight junctions and are subsequently wasted in feces. This would decrease the compromising impact of zonulin by reducing permeability at tight junctions between cells of the protective tissues of the intestine, lungs, blood vessels, and perhaps, the blood barrier. This blockage, if it is achieved, may provide a means of regulating the tight epithelial junctions that create the various protective barriers mentioned earlier. Although he was extremely conservative when discussing the potential benefits of the drug Alba is developing, there can be little doubt that he has considered many more potential applications than I can think to list.
The short-range objective, and the intended market of this drug, is to provide a more rapid and complete disease remission. Although it may ultimately allow a celiac patient to eat a normal diet, this is not the only objective of their development work. I have little personal interest in eating gluten again, but it would be nice not to have to worry about accidental and trace sources of gluten if that is part of what the drug offers. Research has already shown that a gluten-free diet can prevent type I diabetes from developing in two genetically susceptible people. One was at high risk of developing diabetes while the other already had it. This confirms the many animal studies that have shown, among the genetically susceptible, a dose-dependent relationship between gluten ingestion and the development of type 1 diabetes. It is a small leap to infer that if AT-1001 restores the barrier function in the intestinal wall of diabetic patients, as a gluten-free diet does, it should also stop the autoimmune attack on islet cells which make insulin in the pancreas.
The current belief is that when gluten is leaking into the bloodstream and genetically susceptible people mount an immune response against that gluten, the antibodies identify certain sequences of amino acids in the protein structure. These sequences are similar to those found in islet cells, so the antibodies will also attack and destroy these insulin producing cells of the pancreas. By tightening the junctions of the protective barrier in the intestinal wall, thus stopping the leakage of gluten into the bloodstream of genetically susceptible individuals, AT-1001 should also stop the autoimmune result of this process frequently referred to as molecular mimicry. AT-1001 could be used not only to protect surviving islet cells in the type 1 diabetic who still has some production capacity, it can also aid the long-term survival of transplanted islet cells. These transplants are somewhat limited, in current circumstances, because the transplanted cells are destined to be destroyed by the same autoimmune process that destroyed the individual’s original islet cells.
Thus, the therapeutic implications for this drug go far beyond Alba’s short term objectives. Many celiac patients, myself included, experience significant lung disease. I am well aware that my history of smoking cigarettes, now fifteen years in the past, contributed to my lung disease. On the other hand, I’m also aware that when I visit rural locations where there is little air pollution, my lung function improves dramatically.
My own lung problem results, in part, from extensive scarring on the walls of my lungs. This scar tissue impedes the normal exchange of oxygen and carbon-dioxide across the lung wall, to and from the blood. This component of the problem probably won’t get much better. There is also an allergy-driven asthma component to my difficulties. This facet of my lung problems, as shown by my improved lung function, when away from urban air pollution, could be helped dramatically by a drug that tightens the barriers in the lining of my lungs and protects me from the absorption of these airborne particles of pollution.
Zonulin research is so new that it is difficult to predict where it might go, or the medicinal purposes it might serve. Those of us who have been frustrated by watching the medical community overlook the scope and severity of gluten-induced illness may well be vindicated by this work. I had the privilege of speaking to a support group at the University of Arizona Medical School in Tucson last year. At that time I stated that the discovery of zonulin should lead to the Nobel Prize for Fasano et. al. because of the enormous implications of their discovery. The more important outgrowth of this research is that many millions of sick and/or vulnerable people may benefit enormously from AT-1001 if it can be formulated to successfully and effectively regulate the impact of zonulin in humans. It will save and enhance the quality of many lives.








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now