
Celiac.com 01/13/2023 - Celiac disease is an autoimmune disorder in which gluten consumption triggers gut damage. The only effective treatment is a strict gluten-free diet. Can hookworms help celiacs eat gluten? The answer is yes and no, coupled with some trade-offs. Here's the rundown.
Earlier studies have indicated that hookworm infection may restore some level of gluten tolerance in celiac patients, however, none of these approximately one dozen studies were placebo controlled. We've done a number of articles on hookworms and celiac disease. We've even done an article on health claims from at least one hookworm-infected celiac patient who claimed he was able to safely eat gluten.
Can Hookworms Help Celiacs Eat Gluten?
Celiac.com Sponsor (A12):
To get a more detailed answer, a research team recently undertook a randomized, placebo-controlled trial of hookworm infection in nearly sixty people with celiac disease. The team included John Croese, MD; Gregory C. Miller, FRCPA; Louise Marquart, PhD; Stacey Llewellyn, BSc; Rohit Gupta, FRACP; Luke Becker, BAppSci; Andrew D. Clouston, PhD; Christine Welch, FRACP; Julia Sidorenko, PhD; Leanne Wallace, BSc; Peter M. Visscher, PhD; Matthew L. Remedios, FRACP; James S. McCarthy, MD; Peter O'Rourke, PhD; Graham Radford-Smith, PhD; Alex Loukas, PhD; Mark Norrie, PhD; John W. Masson, FRACP; Richard B. Gearry, PhD; Tony Rahman, PhD; and Paul R. Giacomin, PhD.
They are variously associated with the Department of Gastroenterology and Hepatology at The Prince Charles Hospital in Brisbane, Australia; the Center for Molecular Therapeutics, Australian Institute of Tropical Health and Medicine, James Cook University, Cairns, Australia; the Envoi Specialist Pathologists, Brisbane, Australia; the QIMR Berghofer Medical Research Institute, Brisbane, Australia; the Department of Gastroenterology, Townsville University Hospital, Townsville, Australia; the Institute for Molecular Bioscience at the University of Queensland, Brisbane, Australia; the Department of Gastroenterology and Hepatology, Royal Brisbane and Women's Hospital, Brisbane, Australia; the Gastroenterology and Hepatology, Logan Hospital, Brisbane, Australia; and the Department of Medicine, University of Otago, Christchurch and Canterbury District Health Board, Christchurch, New Zealand.
Study Ran Nearly Two Years
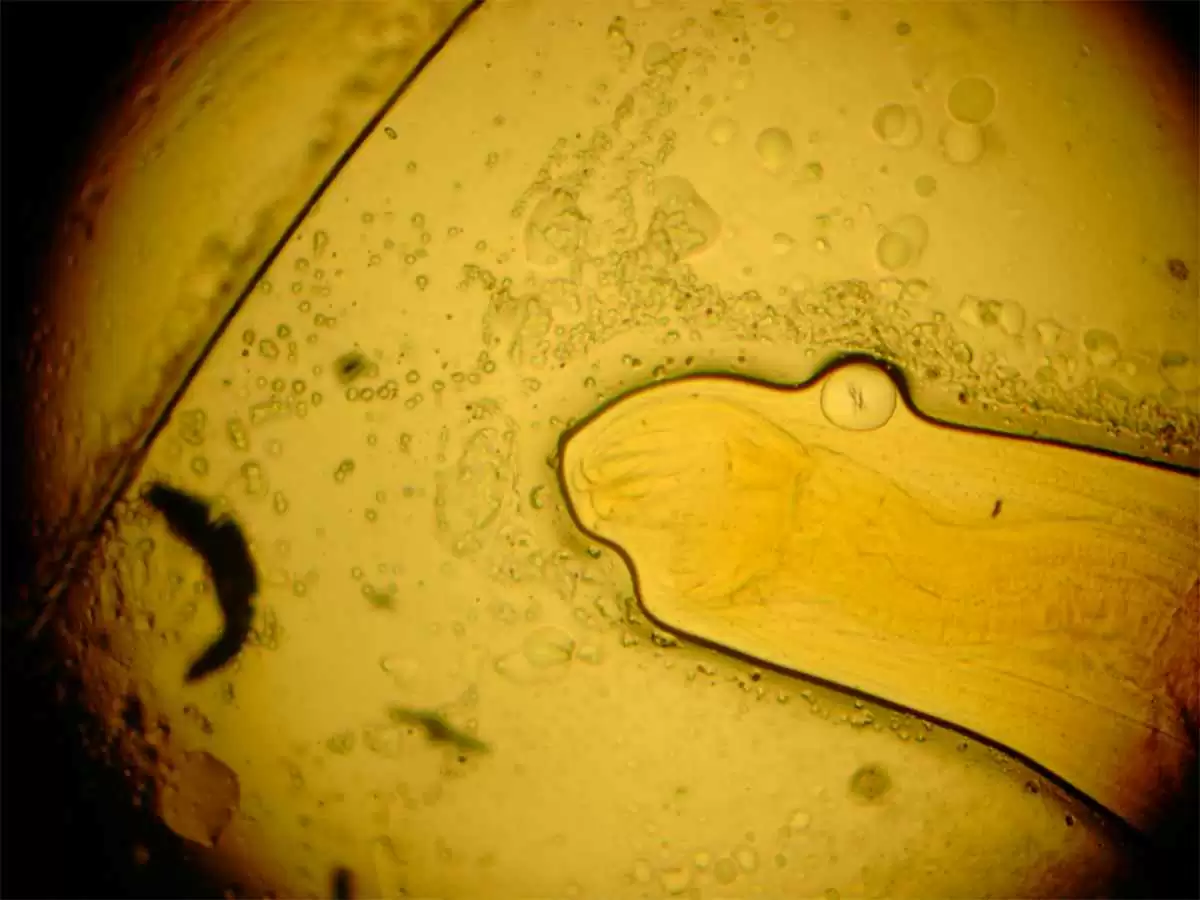
In a study that ran for just under two years, a research team of medical professionals treated celiac patients with with a placebo, or with either third stage larvae of the 20 or 40 Necator americanus hookworm (L3-20 group or L3-40 group).
Patients then increased their gluten consumption to 5 grams per day for 12 weeks, 1 gram intermittent twice weekly for 12 weeks, and two grams sustained for six weeks, followed by liberal diet for 1 year.
About forty to fifty percent of hookworm patients, and about fifty-five percent of placebo subjects made it to the main outcome point of 42 weeks, and hookworm-treated participants did show a sharp reduction in gluten-related events.
Duodenal villous height: crypt depth deteriorated similarly compared with their enrollment values in each group, with an average change of −0.6 for the placebo group; -0.5 for the L3-20 group , −1.1 for the L3-40 group.
A retrospective analysis showed that nearly one in four L3-treated participants failed to develop successful hookworm infection.
Lower Quality of Life Scores for Hookworm Patients
Between forty to fifty percent of participants in each group completed the study, but quality of life symptom scores after the gluten challenge were under forty percent in hookworm-positive participants, compared with over forty-five percent for the hookworm negative group.
From their findings, the team concludes that hookworm infection DOES NOT restore gluten tolerance enough to allow sustained moderate consumption of gluten of two grams per day or more.
However, hookworm infection did lead to better symptom scores after occasional consumption of lower doses of gluten.
The findings undercut the idea that hookworm infection is some kind of magic bullet for gluten consumption for people with celiac disease.
Hookworm Infection Not a Magic Bullet for Celiacs
At best, the data support the idea that hookworm infection can help reduce symptoms of moderate gluten consumption in people with celiac disease, but that any reduction also likely comes with a lower overall quality of life score.
This is the most definitive study we've yet seen on the effects of hookworm infection on the ability of celiac disease patients to tolerate gluten. The results are clear that any modest benefits of hookworm infection comes with some potential reduction in quality of life. Still, the ability of hookworms to help reduce symptoms of moderate gluten consumption in people with celiac disease merits further study.
It's possible that hookworms hold some secrets in their biochemistry that might help to offer some extra protection against the inflammation triggered by limited gluten consumption. That is some exciting news.
Read more at: Clin Transl Gastroenterol. 2020 Dec; 11(12): e00274.



.webp.052ba8c166489209c49990837d6b17e2.webp)



Recommended Comments