
Celiac.com 04/22/2023 - Celiac disease is an autoimmune disorder that may occur in genetically susceptible individuals. It is initiated by ingestion of gluten present in cereals, primarily wheat and to a much lesser extent other cereal proteins such as prolamines of barley and rye. Celiac disease is characterized by malabsorption resulting from inflammatory injury to the small intestinal mucosa. The classical symptoms of celiac disease include diarrhea, weight loss and malnutrition, however, only a small percentage of patients with celiac disease present with classical symptoms. Such patients represent the tip of the iceberg of gluten sensitivity. Many patients with celiac disease may present with short stature, iron and folate deficiency, anemia, bone loss, aphthous stomatitis, arthralgia, and dental enamel defects. Because of the varying and mild clinical presentations, celiac disease is often diagnosed when the patient has grown to adulthood rather than as a child. Adults may present with iron deficiency, anemia, macrocytic anemia and hypocalcemia.
Clinical Presentations of Celiac Disease
Classical
Features Atypical
Chronic Diarrhea
Iron-deficiency anemia
Failure to thrive
Dental enamel defecs
Abdominal distension
Short stature
Osteoporosis/osteopenia
Coexistence with other autoimmune disorders
Celiac.com Sponsor (A12):
Diagnosis based solely on clinical criteria can be misleading and may lead to improper diagnosis and treatment as a result of the variety of clinical presentations often seen in other conditions. Problems with diagnosis has a serious impact on the patient. Delays in diagnosis commonly extend 10-13 years from the first presentation of clinical symptoms, leaving the patient subject to chronic symptoms while searching for proper diagnosis. Failure to diagnose this condition in the short term may predispose an individual to long term complications such as splenic atrophy and intestinal lymphoma. On the other hand, attempts to diagnosis a patient based primarily on clinical criteria may unnecessarily place the individuals on life long gluten-free diet as several transient conditions may mimic celiac disease clinically.
Cancer Morbidity on Normal, Reduced-Gluten and Gluten-Free Diet in Celiac Disease
Diet Group
Number
Observed Malignancies
Expected Malignancies
Observed/ Expected
Excess Morbidity Rate
Normal
46
7
0.19
36.8
10.7
Reduced Gluten
56
5
0.12
41.7
5.0
Gluten-free
108
3
0.46
6.5
1.2
(Howelle PD, Is Coeliac Disease a Pre-Malignant Condition? Gastrointestinal Immunology and Gluten-Sensitive Disease, 1994. p.185)
The true prevalence of celiac disease is difficult to ascertain. However, with the advent of serum antibody methods, incidences as high as one in 300 have been described in the general population, both in Western Europe and in the U.S. celiac disease is prevalent worldwide, but may be rare in individuals of Chinese and Japanese descent.
Prevalence of Celiac Disease
Country
Prevalence based upon Clinical
Prevalence based upon Laboratory
Finland
1:1000
1:330
Italy
1:1000
1:184
Germany
1:2300
1:500
Netherlands
1:4500
1:250
Denmark
1:10,000
1:330
USA
1:10,000
1:250
Guandalini S & Gupta P Clin appl Immun Rev 2:293-305, 2002
Historically, the diagnosis of celiac disease was based primarily on histological studies of the Jejunal biopsy characterized by villous atrophy, crypt hyperplasia, and lymphocytic and plasma cell infiltrate in the lamina propria. Histological examination of the small intestinal biopsy remains the gold standard for diagnosing celiac disease, but has its limitations. Many patients with celiac disease are small children and histological studies may be viewed by many, especially a child’s parents, to be a great discomfort. There may also be problems with accuracy. Occasionally, a biopsy with abnormally high density of intraepithelial lymphocytes with a normal villous architecture may be reported as normal. It has also been reported that some patients with latent or even active celiac disease show normal histopathology (Gastroenterlogy 104:1263-72, 1993). Celiac disease might also be confused with other disorders when diagnosed histologically. Parasitic infections (giardia lamblia) and malabsorption syndrome, for example, may mimic celiac disease histology.
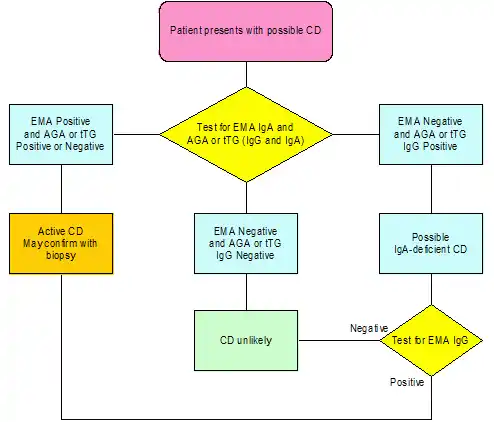
As these limitations have been recognized, serum antibody tests have gained acceptance in screening for celiac disease and in follow-up of patients with celiac disease to determine their compliance to a gluten-free diet. The various serological tests employed in the work-up of patients suspected to have celiac disease include anti-gliadin antibody (AGA), anti-endomysial antibody (EMA), anti-reticulin antibody (ARA) and anti-tissue transglutaminase (tTG) antibody tests. Antibodies to gliadin and tTG are detected by ELISA, whereas endomysium and reticulin antibodies are detected by indirect immunofluorescence. Of the serum antibody tests, EMA and tTG antibody primarily detects antibodies of IgA immunoglobulin isotype, whereas the AGA test detects both IgG and IgA isotypes. No IgM class antibodies to these antigens are detected in patients with celiac disease, hence there is no need to test for IgM class antibodies in the work-up of patients with celiac disease.
Of these tests, AGA was the first to be described in the literature and has been evaluated most extensively. AGA of IgG are more sensitive but less specific then IgA-AGA. The major utility of IgGAGA is in celiac disease patients who are IgA deficient. In a study conducted recently in our laboratory, all of the 15 IgA-deficient celiac disease patients were found positive for IgG-AGA and negative for IgA-AGA and other autoantibodies (Celiac Disease and IgA deficiency: How effective are the serological methods of diagnosis? Clinical diagnostic lab Immunology 9:1295-1300, 2002).
EMA and ARA are very specific indicators of celiac disease. These assays are immuno-histochemical methods and require experience in reading immunofluorescence reactions. Some investigators suggest that they are less sensitive. However, in all the studies conducted since our laboratory first described EMA back in 1983, we find the EMA assay to be 100% specific and sensitive for celiac disease. Other investigators may find EMA to be less sensitive due to the selection of the substrate, fixation of tissue sections, specificity of conjugate employed or serum screening dilution. Internally, we find that testing for EMA at dilutions of 1:2.5 or 1:5 yield 5% of patients positive for EMA yet negative at 1:10 or 1: 20. It could be that some of the investigators who have reported low sensitivity might be screening the patients at high serum dilutions.
Since the identification of tTG as the endomyisal antigen, ELISA methods have been described for detecting antibodies in the sera of patients with celiac disease. The advantage of the anti-tTG antibody assay is that it is an automatable assay that is less subjective than EMA and it is more sensitive and specific than AGA. For these reasons, many laboratories have opted to use the tTG antibody method as the screening method. In these laboratories, it may be the only assay used for detection of celiac disease cases. In the majority of studies of the tTG antibody method, the specificity and sensitivity were found to be between 90-95%. Table 4 on page 15 summarizes the specificity of the AGA, EMA and tTG antibody methods most commonly employed by laboratories performing tests for celiac disease.
Diagnostic Specificity of Serological Markers for Celiac Disease
Assay
Specificity
Sensitivity
Anti-gliadin Antibody IgG
78%
88%
Anti-gliadin Antibody IgA
86%
52%
Anti-endomysial Antibody
100%
100%
Anti-tissue transglutaminase
98%
90-95%
If the prevalence of undiagnosed celiac disease is 4.8 per thousand as reported by Lagerqvist et al (J Intern Med 250:241-48, 2001) then of all the serological methods, EMA is the only method that provides 100% positive and negative predictive value for celiac disease. This raises the question of the optimum method of screening for celiac disease. The answer will vary according to the likelihood of celiac disease in the population studied and upon the experience of the laboratory performing the test. Some investigators may use the AGA or tTG antibody methods for screening and, if positive, confirm using the EMA test. We recommend this approach as it also helps to identify all celiac disease patients, whether IgA-deficient or not.
Celiac disease patients are prescribed a gluten free diet for life. Serological tests are useful in monitoring a patient’s response and adherence to the gluten free diet. The levels of the various antibodies (AGA, EMA, ARA and tTG) decrease and eventually disappear in the majority of the patients on a complete gluten free diet. Similarly, these antibodies either appear or rise in level when the patient is on a gluten containing diet. Serological methods, therefore, play a significant role in both diagnosis and follow-up of celiac disease patients.
Celiac disease has been associated with many other autoimmune disorders such as type 1 diabetes, thyroid autoimmunity and other autoimmune disorders. Approximately five percent of patients with type 1 diabetes have celiac disease. Similarly, approximately the same percentage of patients with celiac disease have type 1 diabetes. It has been proposed that early detection of celiac disease may be beneficial in such cases as it is believed that adherence to a gluten-free diet may delay the onset of diabetes. If true, this further emphasizes the utility of and need for serum antibody tests in the screening of population genetically susceptible for celiac disease.
In conclusion, clinical symptoms of celiac disease are variable and often mild, resulting in significant delays in diagnosis. The use of serological tests has improved the ease of detection, monitoring, and hence— the continuing care of celiac disease patients.







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now