.webp.d58fea91472641c4d2c47a1d94a16be8.webp)
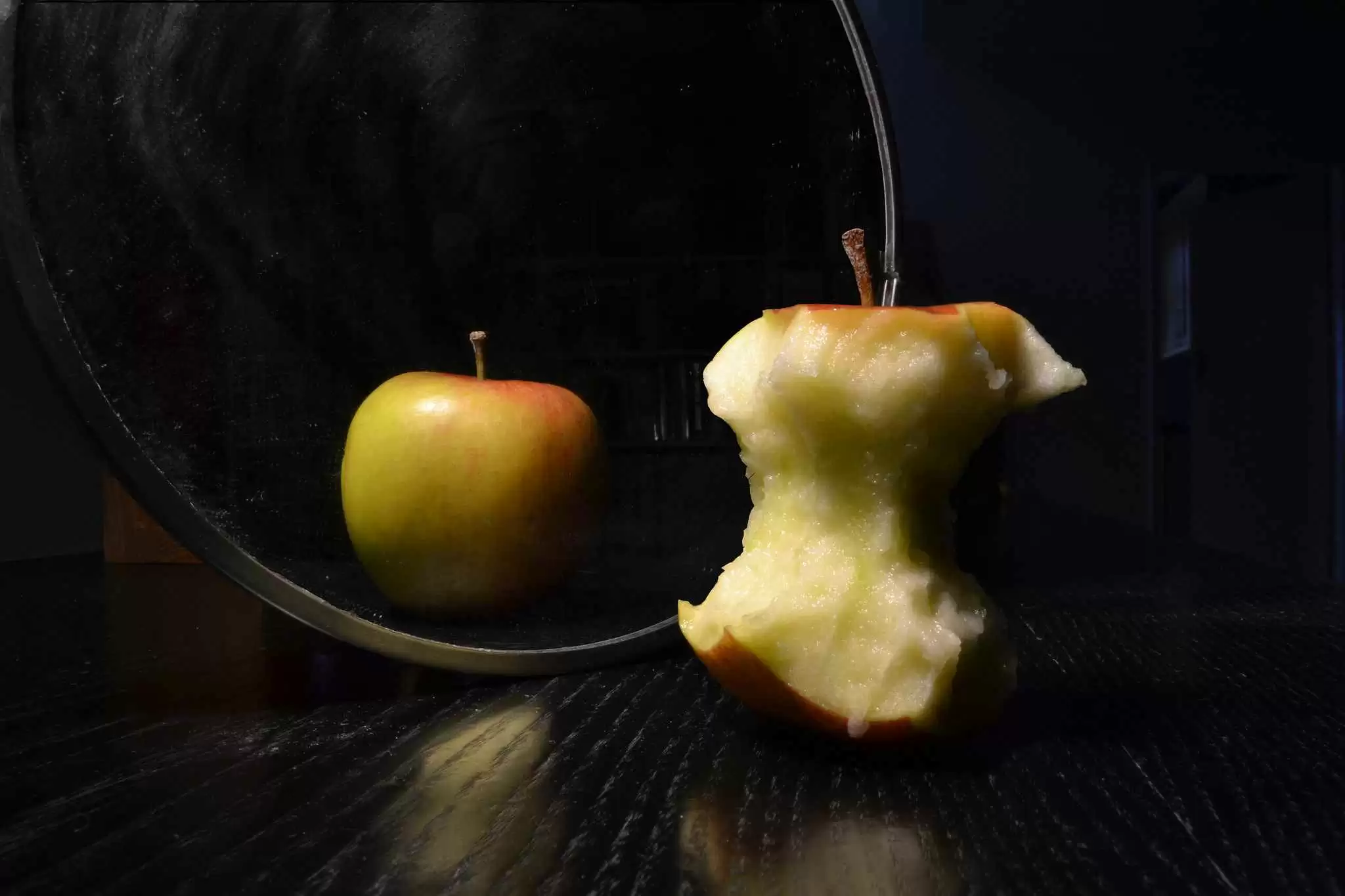
Celiac.com 01/19/2017 - When celiac disease was originally described, one of its hallmark presenting signs was extreme underweight. Along with diarrhea, digestive pain and bloating, the severe weight loss was understood to 'always' be present. Fast forward over 100 years and things have changed. Not only are many celiacs overweight, but those with gluten sensitivity are increasingly falling into that category as well.
Sadly, too often doctors miss testing for these life-long conditions because of a patient's weight status. Stuck in the historical definition, these doctors have missed the current face of celiac and gluten sensitivity – a person can be any weight, and they frequently have weight to lose.
Celiac.com Sponsor (A12):
We often speak of the leaky gut, formally known as a condition of increased intestinal permeability, found in the small intestine. This situation is seen most often in those with an intolerance to gluten due to their upregulation of a protein only made by humans, called zonulin. Zonulin was discovered by Dr. Alessio Fasano and his team.
The zonulin molecule dictates the opening and closing of the 'gates' of the small intestine. With a surface area of over 3,000 square feet, that involves a lot of gates!
While only humans make zonulin, not all humans produce it. Twenty percent do not, 50 percent has a single copy of the gene and 30 percent of the population has both copies of the gene. Those with both copies are in the unenviable position of being two times more likely to die from all causes, and the diseases they do get tend to be more severe.
When a lab test was done on rats highly predisposed to develop type 1 diabetes, two thirds of them never developed the disease when they were given a drug that inhibited zonulin. I know you're going to ask, so here's the answer: A drug does not yet exist for humans that performs this function. However, it is being developed, along with a test for zonulin, by Dr Fasano.
A study published last Fall in Nutrition Research titled "Potential mechanisms for the emerging link between obesity and increased intestinal permeability” and lead by TF Teixeira, found a link that could well explain the obesity issue so commonly seen.
Those with an intolerance to gluten not only tend to have a leaky gut due to the above mentioned zonulin connection, but they also have weakened immune systems due to the constant assault by gluten. The weakened immune system, predominantly housed in the small intestine, is thus less able to defend the body against the normal barrage of bacteria, amoeba, parasites and the like. Why do I call the presence of these organisms 'normal'? Because it is. Now, with that said, it is NOT normal for such organisms to gain a foothold in the intestine and procreate there, but their presence is a normal byproduct of eating food, putting one's fingers in one's mouth, etc. (These are microscopic organisms so don't get too grossed out.) The point is, that a healthy immune system easily kills them; an unhealthy immune system is unable to do its job. The result is a gut full of endotoxins (toxins released from inside bacteria when they disintegrate) or other inhospitable organisms.
These bad organisms thereby fight against the good ones. The good bacteria in the gut (called the microbiome) literally have a population that exceeds the number of cells in the human body by 10 times. The genes associated with this population exceeds that of the human body by 100 times. We are talking about a part of the human body, long under-appreciated, that is now being considered influential enough to be considered an 'organ' in its own right.
Emerging research reveals that when this organ is overwhelmed by toxins in the gut, its composition changes as far as the balance of certain organisms (probiotics), as does its ability to absorb nutrients and expend energy (burn calories). The result is not only weight gain but increased cholesterol, triglycerides, and insulin resistance – the latter leads to diabetes, heart disease and obesity.
Intestinal permeability is also thought to be influenced by a high fat and high fructose diet, plus certain nutritional deficiencies such as zinc.
Another study from the Journal of Parenteral and Enteral Nutrition titled "Gut Microbiota, Intestinal Permeability, Obesity-Induced Inflammation and Liver Injury” found much the same data.
They found that eating a poor diet (high fat, high fructose) could affect the microbiome in as little as one to two days – the result being heart disease and obesity.
So, how do we keep our microbiome happy?
- Discover if you have a gluten or dairy intolerance. If so, avoid those foods.
- Avoid excess, bad fats including fast food, trans fats, preprocessed, prepackaged foods, etc.
- Avoid ALL fructose. I'm not talking about the natural fructose in fruit, of course, but all added fructose, especially high fructose corn sweeteners.
- If you can, get your gut tested for the presence of any inhospitable organisms that have gotten a foothold in your system. This same test will evaluate the health of your microbiome.
- Another test that's good, as a verifier that you're on the right track, is one for a leaky gut. We tend to recommend this one once you've been on a reparative program for a while, to confirm that we are accomplishing our goal.
- Do ingest 9 servings of organic vegetables and fruits each day. These are naturally healing and prebiotic, meaning that they give strength and nourishment to your probiotic population.
- Ensure that you are not deficient in any major vitamins and minerals such as B's, D, zinc, magnesium, calcium, etc.
While it seems like a 'no brainer' to take probiotics, here's a couple of things to keep in mind.
- a. Use a human strain
- b. Get a combination of organisms such as acidophilus, bifidus, etc.
- c. Due to dairy products being such a commonly sensitive food, get probiotics that are free of all dairy.
- d. Sometimes, if you have an infection in the gut, you may feel worse on probiotics. If this occurs, stop them, of course, but realize that you should look into step 4 above. I'm happy to help you!
Don't cheat. I'm sorry, but being 'good' Monday through Friday and going crazy on the weekends just isn't going to cut it if you want to be healthy. And if your health is already compromised somewhat, cheating just isn't worth the dangerous repercussions. That microbiome can change in a day or two when you've been eating a poor diet. Remember that.
I hope you found this helpful. It is interesting how much we are discovering about how the health of the gut dictates so much about our general health or tendency towards disease. And it's also quite revealing how much of a culprit gluten can be when trying to optimize the function of the small intestine and its immune system.
Please send me your questions or comments. I am here to help!
My clinic, HealthNOW Medical Center, is a destination clinic. You don't need to live locally to receive help with your health. You are welcome to call us anytime for a free health analysis – 408-733-0400.
References:
- Nutrition Research. 2012 Sep;32(9):637-47. Potential mechanisms for the emerging link between obesity and increased intestinal permeability.Teixeira TF, Collado MC, Ferreira CL, Bressan J, Peluzio Mdo C.
- Journal of Parenteral and ENteral Nutrition 2011. Gut Microbiota, Intestinal Permeability, Obesity-Induced Inflammation and Liver Injury. Thomas H. Frazier, MD1; John K. DiBaise, MD, and Craig J. McClain, MD. Volume XX Number X









Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now