Celiac.com 09/30/2024 - This study explores how specific dietary components like fructo-oligosaccharides and gluten affect the gut health of individuals who report non-celiac gluten sensitivity (NCGS). NCGS is characterized by gastrointestinal symptoms similar to celiac disease but without the autoimmune response or intestinal damage that defines celiac. Researchers aimed to understand how these components impact the gut microbiota, focusing on specific bacterial populations, inflammation markers, and fermentation by-products. By comparing these effects with a placebo, the study hoped to clarify the roles of gluten and fructans in gut health for those with NCGS.
The study aimed to shed light on how these dietary elements influence the gut microbiota, focusing on specific bacterial populations, inflammatory markers, and fermentation by-products, while comparing these effects to a placebo. Through this research, the team hoped to better understand the roles of gluten and fructans in gut health, especially in those without a formal celiac diagnosis.
Study Design and Participants
Celiac.com Sponsor (A12):
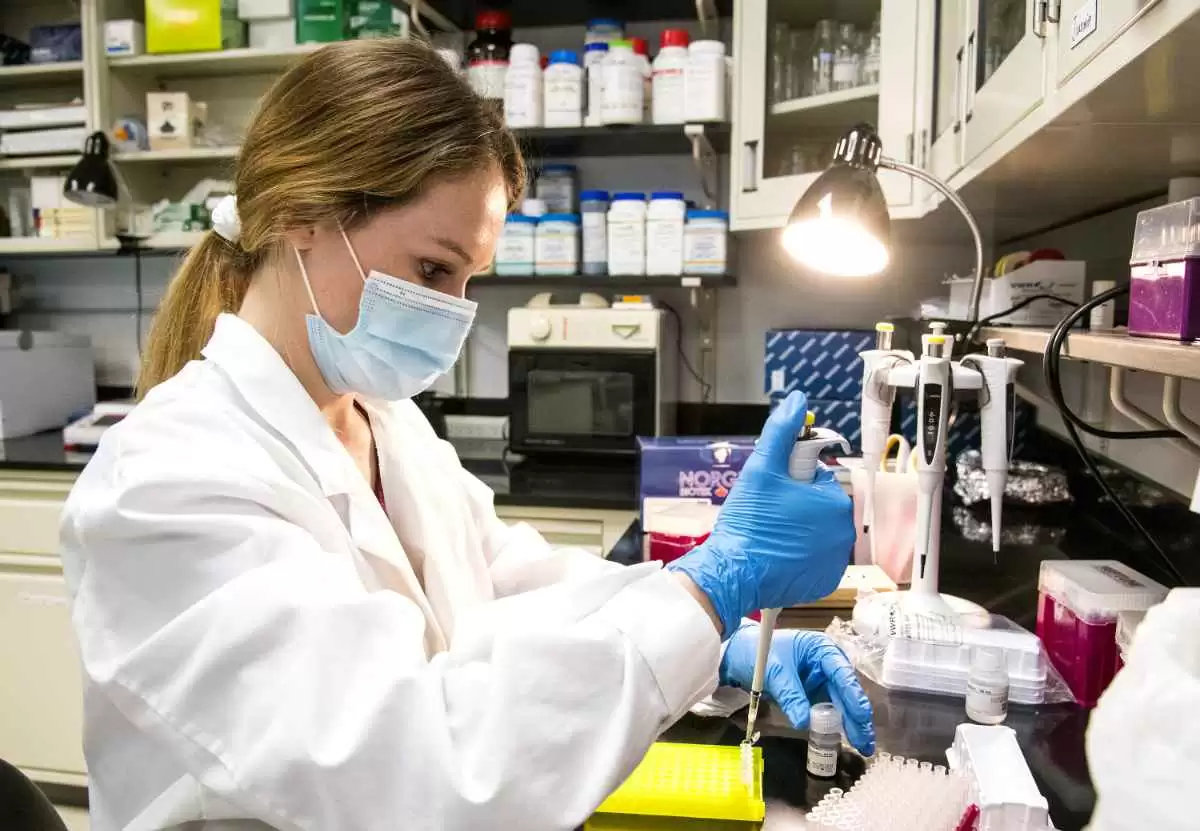
The researchers conducted a double-blind, randomized controlled crossover trial. The participants were 59 individuals who reported relief from gastrointestinal symptoms when following a gluten-free diet but did not have diagnosed celiac disease. All participants were required to maintain a gluten-free diet for at least six months before joining the study.
During the trial, participants were subjected to three different seven-day dietary challenges: consuming gluten (5.7 grams per day), fructo-oligosaccharides (2.1 grams per day), or a placebo. These challenges were administered in a randomized sequence, with each challenge followed by a washout period to ensure that participants' symptoms returned to baseline levels before the next test.
The study primarily sought to determine how these dietary elements influenced gut microbiota composition, microbial fermentation, and the presence of specific gut inflammation markers. Researchers used stool samples from participants to analyze changes in bacterial populations, short-chain fatty acids (a product of microbial fermentation), and inflammation markers like lipocalin 2, a biomarker of gut inflammation.
Key Findings on Gut Microbiota
The effects of fructans and gluten on the gut microbiota varied significantly. In participants who consumed fructans, there was a notable increase in certain bacterial taxa, such as Fusicatenibacter, while other groups like Eubacterium coprostanoligenes and Anaerotruncus showed a decrease. The changes in gut microbiota in response to gluten were less pronounced, with a slight increase in bacteria from the Eubacterium xylanophilum group.
Interestingly, the diversity of the microbiota, both in terms of species richness and overall structure, remained unchanged across all challenges. This suggests that while certain bacterial populations were affected by the diet, these shifts did not dramatically alter the overall composition of the gut's microbial community.
One notable finding was the association between the reduction of Eubacterium coprostanoligenes after fructan consumption and the increase in gastrointestinal pain. This bacterial group may play a role in protecting against discomfort, and its decrease could potentially explain some of the symptoms experienced by participants.
Gastrointestinal Symptoms and Their Association with Bacteria
Fructans were more likely than gluten to cause gastrointestinal discomfort in the participants. However, these symptoms were not directly associated with significant changes in the overall gut microbiota composition. This suggests that the gastrointestinal symptoms experienced by participants after consuming fructans were not necessarily driven by major shifts in the microbial population but rather by more subtle or localized effects on certain bacterial groups.
The baseline composition of the gut microbiota also appeared to influence how participants responded to both fructans and gluten. Those who had specific bacterial profiles before the challenges tended to have different symptom experiences, implying that individual microbiota makeups may determine how sensitive a person is to particular dietary components.
Inflammatory Markers and Short-Chain Fatty Acids
Despite the changes observed in specific bacterial populations, the study found no significant differences in inflammatory markers or the production of short-chain fatty acids between the diet challenges. The levels of lipocalin 2, the inflammation marker, remained steady regardless of whether participants consumed fructans, gluten, or the placebo.
The concentration of short-chain fatty acids, which are produced by the fermentation of dietary fibers in the gut, also did not show notable variations across the different dietary challenges. This could be because the doses of fructans used in the study were relatively low, and a longer intervention period or higher dose might be needed to observe significant changes in these metabolites.
Conclusion and Relevance for Individuals with Celiac Disease
The findings of this study suggest that fructans may trigger more gastrointestinal symptoms than gluten in individuals with non-celiac gluten sensitivity. However, the study did not uncover substantial shifts in the overall composition of the gut microbiota that could explain these symptoms. Instead, it points to the possibility that individual variations in gut microbiota at baseline may influence how people respond to dietary fructans and gluten.
For individuals with celiac disease or non-celiac gluten sensitivity, this study highlights the importance of considering not only gluten but also other dietary components like fructans, which may contribute to gastrointestinal symptoms. Although this study focused on people without diagnosed celiac disease, its insights could guide further research into how diet and gut bacteria interact in those with diagnosed gluten-related disorders.
In conclusion, the study offers valuable insights into the complex relationship between diet, gut bacteria, and gastrointestinal health. While more research is needed to fully understand these mechanisms, the findings emphasize the role that individual differences in microbiota composition may play in dietary sensitivities, which could be crucial for tailoring personalized treatment approaches in the future.
Read more at: biomedcentral.com








Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now