Celiac.com 05/12/2022 - Recent studies suggest that KIR+CD8+ T cells could offer a path to controlling autoimmune diseases, such as “long COVID,” which emerge after viral infections.
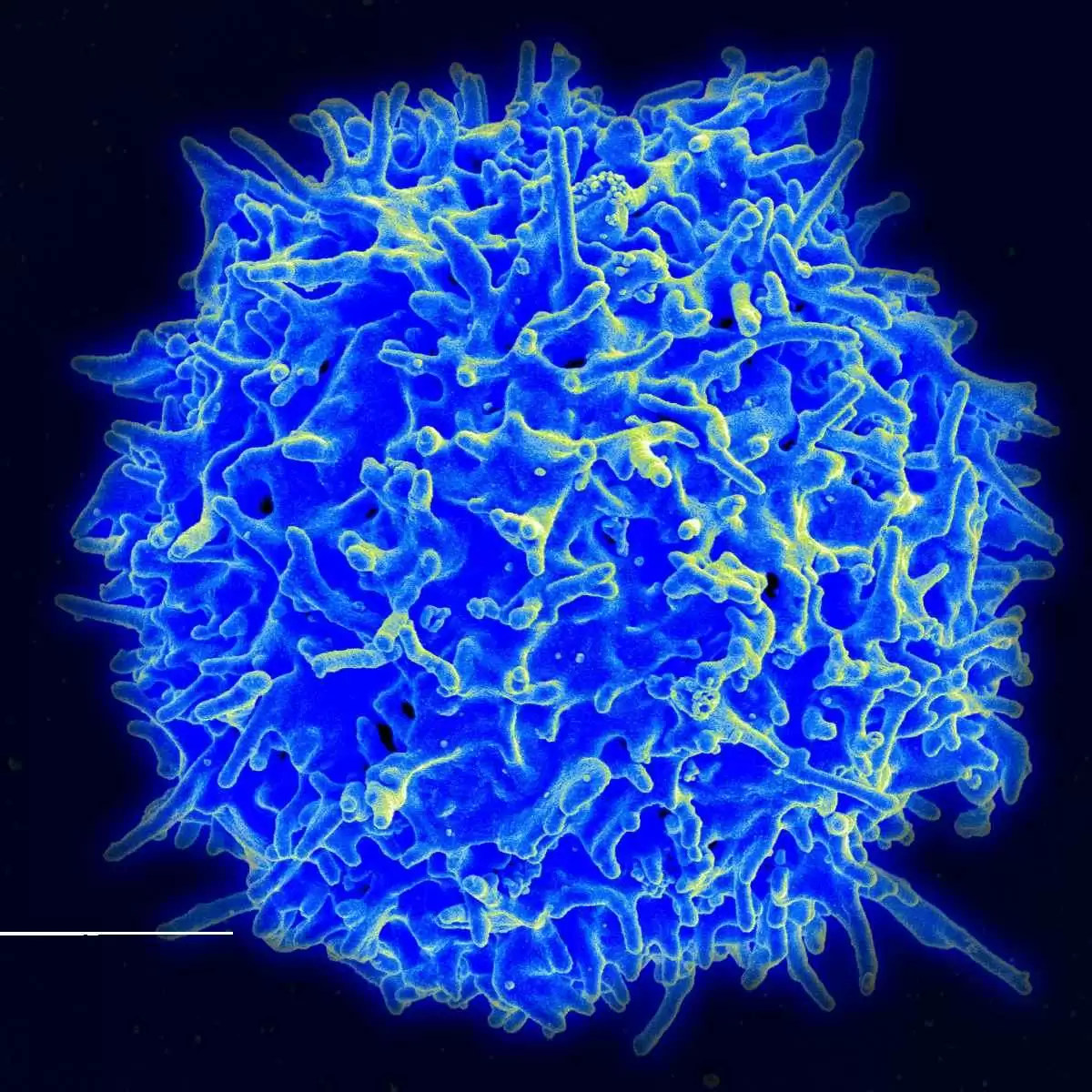
Ly49+CD8+ T cells are a subset of CD8+ T cells that have shown immunoregulatory activity in mice. These cells can suppress myelin oligodendrocyte glycoprotein (MOG)–specific pathogenic CD4+ T cells through their cytolytic activity and thereby ameliorate experimental autoimmune encephalomyelitis (EAE).
Celiac.com Sponsor (A12):
However, whether a similar CD8+ regulatory T cell subset exists in humans and whether its suppressive activity extends beyond autoimmune diseases to play a more general role in peripheral tolerance remains to be determined.
A team of researchers recently shared some relevant findings regarding CD8+ T cells in humans.
The research team included Jing Li; Maxim Zaslavsky; Yapeng Su; Jing Guo; Michael J Sikora; Vincent van Unen; Asbjørn Christophersen; Shin-Heng Chiou; Liang Chen; Jiefu Li; Xuhuai Ji; Julie Wilhelmy; Alana M McSween; Brad A Palanski; Venkata Vamsee Aditya Mallajosyula; Nathan A Bracey; Gopal Krishna R Dhondalay; Kartik Bhamidipati; Joy Pai; Lucas B Kipp; Jeffrey E Dunn; Stephen L Hauser; Jorge R Oksenberg; Ansuman T Satpathy; William H Robinson; Cornelia L Dekker; Lars M Steinmetz; Chaitan Khosla; Paul J Utz; Ludvig M Sollid; Yueh-Hsiu Chien; James R Heath; Nielsen Q Fernandez-Becker; Kari C Nadeau; Naresha Saligrama; and Mark M Davis.
A recent report by Li et al., notes the existence of a similar CD8+ T cell subset in humans, which possess killer cell immunoglobulin-like receptors (KIRs). This function in humans mirrors that in the mouse Ly49 family.
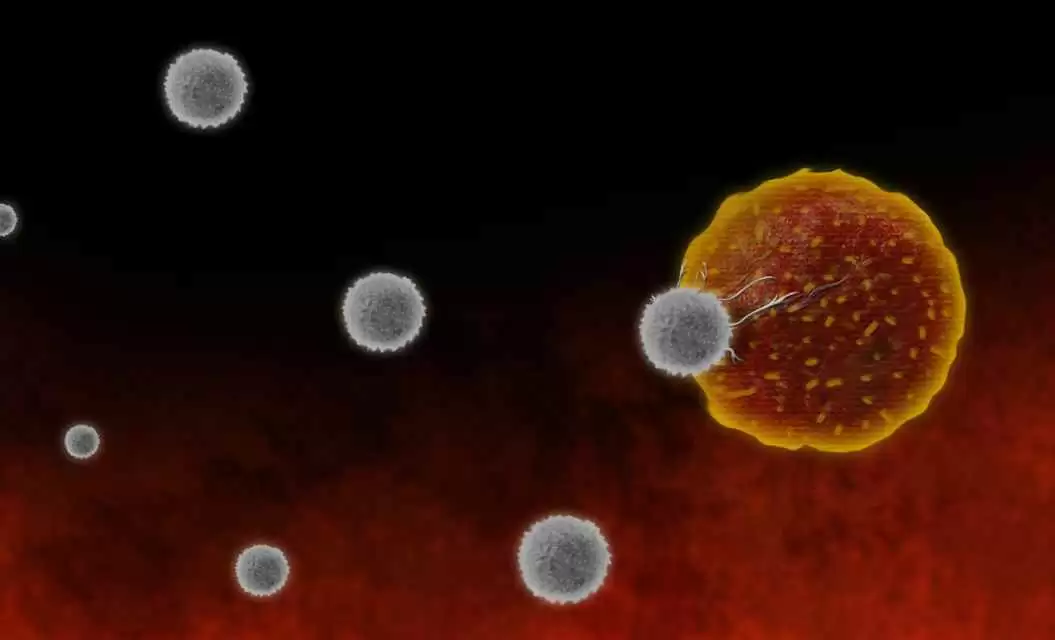
These cells are able to suppress self-reactive CD4+ T cells, and are more plentiful in patients with autoimmune conditions, such as celiac disease, multiple sclerosis, and lupus, as well as in patients infected with influenza virus or severe acute respiratory syndrome coronavirus 2.
When researchers injected viruses into mice selectively deficient in Ly49+CD8+ T cells, the mice showed normal antiviral immune responses, but they later developed symptoms of autoimmune disease.
The team found that CD8+ T cells express inhibitory killer cell immunoglobulin-like receptors (KIRs), making them the human equivalent of Ly49+CD8+ regulatory T cells in mice.
These CD8+ T cells are abundant in the blood and inflamed tissues of patients with several different autoimmune diseases. Moreover, these CD8+ T cells easily eliminated pathogenic gliadin-specific CD4+ T cells from the leukocytes of celiac disease patients in vitro.
Because of this, KIR+CD8+ T cells could offer a path to controlling autoimmune diseases, such as “long COVID,” which emerge after viral infections.
Tellingly, in COVID-19 patients, the team also found elevated levels of KIR+CD8+ T cells, but not CD4+ regulatory T cells, which corresponded to disease severity, and levels of vasculitis.
Selective destruction of Ly49+CD8+ T cells in virus-infected mice reversed their infections, and restored their autoimmunity.
These results suggest that in humans, as in mice, these regulatory CD8+ T cells act uniquely to suppress pathogenic T cells in autoimmune and infectious diseases.
Read more in Science. 2022 Apr 15;376(6590):eabi9591.
Also: PubMed.
The researchers are variously affiliated with the Institute of Immunity, Transplantation and Infection, Stanford University School of Medicine, Stanford, CA, USA; the Program in Computer Science, Stanford University, Stanford, CA, USA; the Institute for Systems Biology, Seattle, WA, USA; the Department of Microbiology and Immunology, Stanford University School of Medicine, Stanford, CA, USA; the Department of Genetics, Stanford University School of Medicine, Stanford, CA, USA; the KG Jebsen Coeliac Disease Research Centre, University of Oslo, Oslo, Norway; the Institute of Clinical Medicine, University of Oslo, Oslo, Norway; the Department of Immunology, University of Oslo, Oslo, Norway; The Howard Hughes Medical Institute, Stanford University School of Medicine, Stanford, CA, USA; the Human Immune Monitoring Center, Stanford University School of Medicine, Stanford, CA, USA; the Department of Chemistry, Stanford University, Stanford, CA, USA; Sean N; Parker Center for Allergy and Asthma Research, Department of Medicine, Stanford University, Stanford, CA, USA; the Program in Immunology, Stanford University School of Medicine, Stanford, CA, USA; Division of Neuroimmunology, Department of Neurology and Neurological Sciences, Stanford University School of Medicine, Stanford, CA, USA; the Department of Neurology and UCSF Weill Institute for Neurosciences, University of California, San Francisco, CA, USA; Department of Pathology, Stanford University School of Medicine, Stanford, CA, USA; VA Palo Alto Health Care System, Palo Alto, CA, USA; the Division of Immunology and Rheumatology, Department of Medicine, Stanford University, Stanford, CA, USA; the Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA; the Stanford Genome Technology Center, Stanford University, Palo Alto, CA, USA; the European Molecular Biology Laboratory (EMBL), Genome Biology Unit, Heidelberg, Germany; the Department of Chemical Engineering, Stanford University, Stanford, CA, USA; the Stanford ChEM-H, Stanford University, Stanford, CA, USA; the Department of Immunology, Oslo University Hospital, Oslo, Norway; the Department of Bioengineering, University of Washington, Seattle, WA, USA; and the Division of Gastroenterology and Hepatology, Department of Medicine, Stanford University, Stanford, CA, USA.


.webp.c53b640f544ac5b6827ea9b8bf621ae6.webp)




Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now