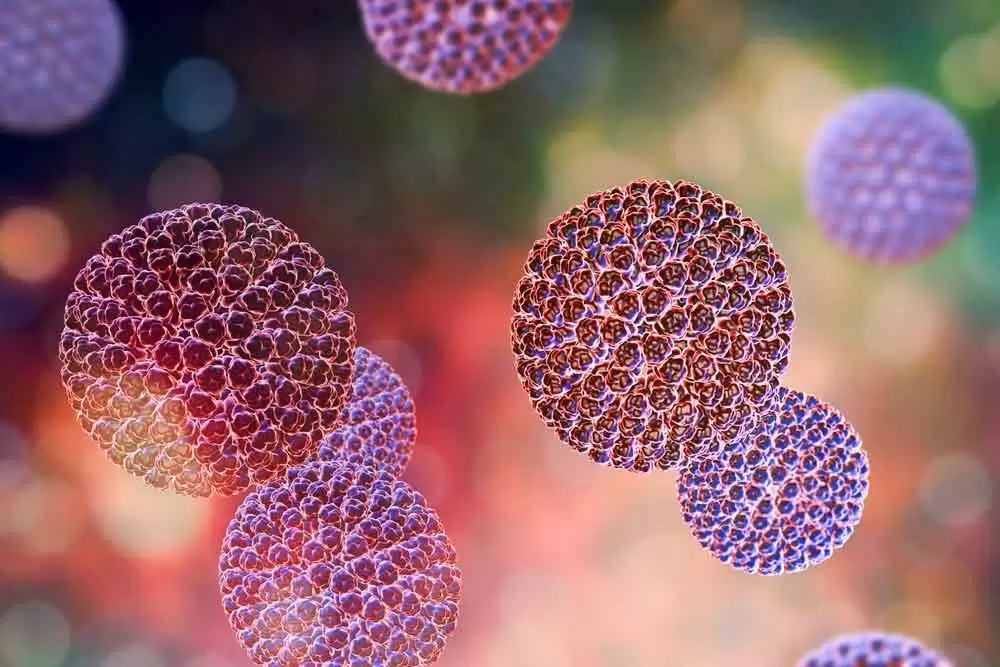
Celiac.com 03/20/2019 - Sensitivities to gluten are becoming more common. Patients with celiac disease have wheat-specific immune responses, but researchers have remained uncertain about the potential role of non-wheat proteins in triggering symptoms in celiac or gluten-sensitive patients.
A team of researchers recently set out to assess the role of non-gluten proteins that may trigger symptoms in celiac or gluten-sensitive patients. Specifically, the team wanted to determine if lactobacillus degrades and/or reduces the inflammatory effects of amylase trypsin inhibitors (ATI).
Celiac.com Sponsor (A12):
The research team included Alberto Caminero, Justin L. McCarville, Victor F. Zevallos, Marc Pigrau, Xuechen B. Yu, Jennifer Jury, Heather J. Galipeau, Alexandra V. Clarizio, Javier Casqueiro, Joseph A. Murray, Stephen M. Collins, Armin Alaedini, Premysl Bercik, Detlef Schuppan, and Elena F. Verdu.
The researchers put mice on a gluten-free diet, with or without wheat amylase trypsin inhibitors (ATI), for one week. Mice included a control group of C57BL/6 mice, and groups of Myd88–/–, Ticam1–/–, and Il15–/– mice. The team then collected small intestine tissues and measured intestinal intraepithelial lymphocytes (IELs). They also looked at gut permeability and intestinal transit times.
Control mice fed ATI for one week were fed daily with Lactobacillus strains with either high or low ATI-degrading capacity. The team sensitized NOD/DQ8 mice to gluten, and then fed them an ATI diet, a gluten-containing diet or a diet with ATI and gluten for two weeks. Mice were also treated with Lactobacillus strains that had high or low ATI-degrading capacity. The team took samples of intestinal tissues, and measured IELs, gene expression, gut permeability and intestinal microbiota profiles.
Intestinal tissues from control mice show that ATI triggered an innate immune response by activating TLR4 signaling to MD2 and CD14, and impaired barrier function even in the absence of mucosal damage.
Gluten-sensitized mice carrying HLA-DQ8 showed increased intestinal inflammation in response to dietary gluten. The team found that lactobacillus degraded and reduced the inflammatory effects of ATI.
In conclusion, amylase trypsin inhibitors influence gluten-induced intestinal symptoms in wild-type mice and increase inflammation to gluten in genetically susceptible mice. Lactobacillus degrades and reduces the inflammatory effects of ATI.
Strategies to alter the gut microbiome, such as the ingestion of bacteria that can degrade and reduce ATI, may be helpful for people with various wheat-sensitivities, including celiac disease.
Read more at Gastroenterology
The researchers are variously affiliated with the Farncombe Family Digestive Health Research Institute, McMaster University, Hamilton, Ontario, Canada; the Research Center for Immunotherapy, University Medical Center, Johannes Gutenberg University, Mainz, Germany; Institute of Translational Immunology, University Medical Center, Johannes Gutenberg University Mainz, Mainz, Germany; the Department of Medicine, Columbia University, New York, NY, USA; the Institute of Human Nutrition, Columbia University, New York, NY, USA; the Department of Microbiology. Universidad de Leon, Leon, Spain Division of Gastroenterology and Hepatology, Department of Immunology, Mayo Clinic College of Medicine, Rochester, Minnesota; the Research Center for Immunotherapy, University Medical Center, Johannes Gutenberg University, Mainz, Germany; Institute of Translational Immunology, University Medical Center, Johannes Gutenberg University Mainz, Mainz, Germany; and the Division of Gastroenterology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA.






Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now