
Celiac.com 09/13/2016 - Six times from 2003 – 2005, I had a mysterious full-bodied, itchy, blistery rash that landed me in the emergency room the first time, where seven doctors shook their heads. The ER physicians agreed that it was a "systemic chemical reaction" and tried to identify what I could have been exposed to. A dairy allergy was ruled out immediately since I have been completely dairy-free for twenty years. For the next three years, between hiding from the world for the ten days of intense itching and for the six weeks it took my skin to heal after an outbreak, I saw numerous dermatologists, internists, gastroenterologists, allergists and chiropractors. No one could figure out what was causing this miserable rash.
I finally met the "best diagnostician" according to Denver's 5280 Magazine who told me he would figure out what was causing my plight, but that it wouldn't be fun. At that point, I was willing to take any test to identify what my enemy was. I endured ninety-eight needle sticks (who's counting?) eight skin biopsies, invasive scopes and tests for allergies, rheumatoid arthritis, diabetes, thyroid disease and a host of other procedures. The skin biopsies erroneously concluded that I had scabies. Scabies are biting mites that leave bumps on the skin. It couldn't have been mites, because my husband, who lives in the same environment, didn't have a bump on his body.
Celiac.com Sponsor (A12):
There was only one test that I did not pass – elevated levels of IgG antibodies in my blood. My doctor suggested that the rash could be correlated with gluten consumption and recommended that I try a gluten free diet. After being vigilant for several months, five out of seven long-term chronic complaints, including the rash, gradually went away.
Here's my understanding of the DH lifecycle. An intestine that cannot break down the protein gluten leaks it out of the intestine and into the bloodstream. The blood sees this as a foreign protein and over-produces the immunoglobulin G to attack it. The antibodies build up, and purge out through the skin causing the rash. Completely avoiding gluten eliminates the antibody buildup, and the rash. One clue that might have streamlined my diagnosis is the knowledge that the DH rash is symmetrical. If it appears on one elbow, it will appear on the other, etc. In my case, it appeared on both sides of my entire body from the neck down.
Please understand, I am not a doctor and the following is not to be considered medical advice. I am sharing this to pass along a few things I've learned from personal experience, research and lectures on the subject with the hope of helping others who suffer from a chronic, pervasive, itchy rash.
Initial Testing
Since I had the eight skin biopsies, I've learned that immunofluroescent biopsies should have been taken of the healthy skin near the rash rather than of the actual bumps. I was never given this test.
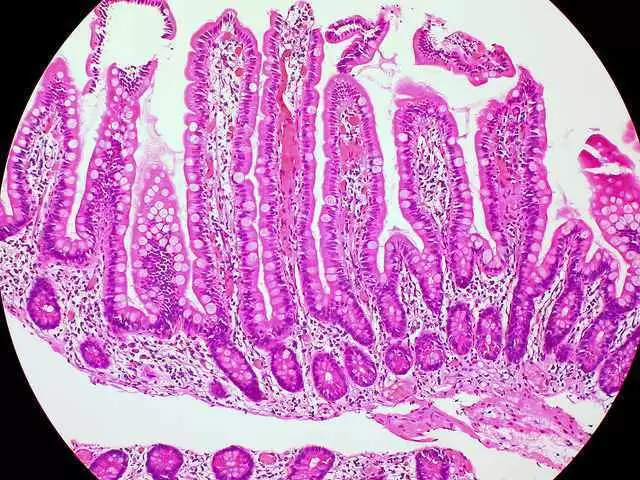
After all those tests, the elevated IgG was the only indication that gluten is the culprit. I endured what was considered the "gold standard" for diagnosing celiac disease, the upper GI scoping, and my gastroenterologist did not find any damage. I have since learned that the upper GI scoping is no longer thought to be the "gold standard" diagnostic process by many celiac experts because it is too random. If the doctor doesn't biopsy the intestines in exactly the right place, you may be deemed to be celiac-free when you actually have considerable intestinal damage several inches away from the biopsy site. Furthermore, people with DH may or may not experience damage to their small intestine. A study done in 2010 found that 67 percent of the time people with DH only have elevated IgG-TGA levels (1).
My doctor divulged that there simply are not yet 100 percent conclusive tests for celiac disease. He said that the best way to be sure of the diagnosis is to observe that the chronic symptoms disappear over time by vigilantly following a gluten free diet.
Residual Rashes
Residual rashes can reappear for up to five years even though the person is following a gluten free diet. The accumulated antibodies purge in a histamine response (the rash) periodically through the skin. Horrible as an outbreak is, the rash is actually how the body cleanses itself of the antibodies. The good news is, rashes diminish in time with strict adherence to a gluten free diet.
Ongoing Testing
I've learned that the best way to monitor the healing process is to have the IgG antibodies tested once a year until they are in the normal range. The number should decline each year, which implies compliance to the gluten free diet and that residual rashes will diminish. Mine took several years to finally reach the normal range. Having IgGs in the normal range does not mean that I can ever go back to eating gluten. DH is a life-long condition controlled by a gluten-free, and often, a dairy-free diet. Some studies talk about a spontaneous remission. This is very rare.
Other Triggers
People who have a propensity to develop rashes need to be aware of other triggers.
- Iodine triggers the rash in people with DH. Seaweed, shellfish, especially shrimp and lobster should be avoided. Sushi wrapped in Nori seaweed has caused me to have an outbreak before. Watch out for thyroid medicine and water filters because both can contain iodine.
- Sunburns can cause rashes. If your skin is sensitive enough to get a rash, chances are, sun will irritate it and could trigger an outbreak. Stay in the shade, wear translucent zinc oxide sunscreen and avoid too much exposure.
- An overgrowth of Candida (yeast) can cause an outbreak. Candida is naturally present in the body. To avert an overgrowth, eliminate simple sugars from the diet. According to a study done at Rice University, 70 percent of the population have an overgrowth of Candida somewhere in their body(2) due to over-exposure to antibiotics, steroids and hormones.
- Women who are "estrogen dominant" may not be producing progesterone. This can happen during perimenopause and in menopause. According to the book What Your Doctor May Not Tell You About Menopause by John R. Lee and Virginia Hawkins(3), estrogen dominance causes autoimmune and histamine reactions in some people. This could be the reason that women who have eaten gluten for years without symptoms are suddenly are plagued when they are in their 40's or 50's.
- Pharmaceuticals can trigger rashes in people with DH. If there is a choice of two drugs and one says a side effect may be a rash, and a similar drug doesn't, opt for the one that doesn't say "rash" for a side effect.
- Inadvertent gluten consumption can also cause the rash. Gluten is in nearly every processed food, and in many cosmetics and drugs. Some mushrooms are even grown on gluten! Transglutaminase enzymes are used to revive aging fish and meats – to extend their shelf life and to make them look appetizing. Grocers do not have to declare that they add these enzymes because they are naturally occurring in the human body. Dr. Peter Green mentioned at a Gluten Intolerance Group conference that people with celiac disease develop antibodies to tissue transglutaminase, and that the addition of those enzymes may be causing people who are already sensitive to get sicker. The point is that even foods that are supposedly gluten free can contain small amounts of it. To be safe, test products with ELISA test strips. ELISA test strips are available at Open Original Shared Link. Since these strips are so expensive, this is also a website for everyone who uses them to post their results. I have learned a lot by reading this forum.
Day-to-Day Life
The longer I have been gluten free, the less tolerant my body has become. I've heard this anecdotally from others following the gluten-free diet. My DH is so severe, I react to even the most minor infractions. It makes eating out very difficult because cross-contamination is common and waiters are not always aware. I have a little test for waiters to decide whether to trust them to bring me a ‘safe' meal. I order a club soda with lemon before I order food. If the soda comes with lime, I know this waiter is not listening, and will be more likely to bring me something that could contain gluten. In restaurants that flunk my club soda test, I play it safe and order salad, a fruit plate or steamed vegetables.
I've been to restaurants that tout a gluten free menu, only to be presented with a laminated disclaimer saying they are not liable for cross-contamination or inadvertent gluten after I order. How can anyone enjoy a meal with that kind of disclaimer? Not to mention the disruption of the conversation with your meal-mate when presented with a disclaimer card. It can be a little embarrassing!
The most frustrating aspect of living with this is when accidental infractions occur. In November 2011, I wasn't feeling very well, so I took an aspirin and went to bed. Ten days later, the rash started appearing. It was a very bad rash, and I had to wear gloves to cover my hands that had doubled in size. I could not figure out what I had consumed that had gluten in it. My home is gluten free! I thought perhaps a product that I habitually used changed ingredients, so I read all the ingredients of everything in my house. Using the ELISA test strips, I tested 44 different products – foods, pharmaceuticals, over-the-counter drugs, cosmetics – everything that came in contact with my skin, or that I ate. Nothing I tested contained gluten. Then I remembered taking the aspirin. I tested it, and it contained gluten! I read the ingredients, the label said "Inactive ingredient: starch." It did not say what kind of starch. This happens in binders in pharmaceuticals too. The ingredients of pharmaceuticals will say "starch #3," and further investigation reveals this can alternate between wheat, tapioca, corn or potato. This means every time a prescription is refilled, it must be tested to be sure that particular batch wasn't made with wheat starch.
I was in a car wreck and had to be taken to the emergency room. My sternum was broken, and I needed pain medication. The nurse offered me a pill and I asked if they would please make sure that it was gluten free. The nurse said, "pharmaceuticals are gluten free." (I've had pharmacists tell me this too – but as mentioned above, it is not true!) I said, "The reaction I get from consuming gluten is worse than the pain of this broken bone. Would you mind checking?" The nurse came back 30 minutes later and told me the pill did, indeed contain gluten. I went home in the middle of the night without any pain medication. I found a website the next morning that lists all gluten free pharmaceuticals, and asked my doctor to call in the specific brand of pain medication. The website is Open Original Shared Link. I have learned to keep a bottle on hand at home, and when I travel in case something like that ever happens again.
I really wanted to eat the gluten free oats, so in 2009, I decided to go completely grain free for three months to cleanse myself for the "oat challenge." Then I made some oatmeal cookies with the gluten free oats. I took one bite, and waited ten days. Sure enough, the rash appeared on my legs. Through this experiment, I learned that I am not tolerant of even some "gluten free" foods.
Through my studies of alternative diets and trying to discover the optimal way to eat to improve health, I have learned that a diet centered on eating vegetables, fruits, beans and some nuts and seeds improve the autoimmune system. Once the immune system is restored, (after strict adherence for several years), I've been told that it may be possible to undergo gluten desensitization under doctor's supervision. Locating a credible doctor to do this may be tricky, and deliberately exposing myself to gluten would take a lot of courage. However, I am considering this down the road with the hope that if I am inadvertently exposed to tiny amounts of gluten, I won't suffer through another rash.
Since my reaction is so severe, I asked my doctor to write an undated letter on his letterhead "To Whom It May Concern" that states my reaction to gluten. I take this with me whenever I travel, just in case I was ever hospitalized, I could show the staff a letter from a bona fide medical doctor stating the severity of my situation. Without a letter, I am not sure if anyone would adhere to the strict gluten free guidelines I need to follow.
Rash Remedies
In those dismal three years before I was diagnosed, I was given mega doses of steroids, antibiotics, antihistamines, countless prescription creams, gels, histamine blocks, anti-viral drugs, anti-fungals and offered Dapsone. Since it took years to diagnose, well-meaning doctors offered a smattering of drugs to see what might work.
Most of the drugs listed above were not the right medicine for DH. Steroids proved ineffective. Antivirals and antifungals did not work either. Dapsone is commonly given to people with DH who are not able to adhere to a gluten free diet. It is a strong drug originally given to lepers and has severe side effects. I'd rather live the gluten free lifestyle than take Dapsone.
Once diagnosed, the two drugs that worked for me to ease symptoms for outbreaks were Zantac and liquid Hydroxizine. I am told that Zantac is a histamine block. It helped to reduce the number of itching days from ten to eight. I was also told to take it as precaution, if I felt I had inadvertently eaten gluten to thwart off an outbreak. I took the liquid hydroxizine around 4:00 o'clock in the afternoon when the histamines are highest, to ease the itching through the night. An un-exotic over-the-counter remedy that works is the clear calamine lotion from Walgreen's. There were days that I dreamed of taking a bath in that wonderful stuff!
Another remedy recommended by a DH friend is a product made by Bayer called Domeboro Astringent Solution. It is a powder that is mixed with water and applied with a cloth to the affected area. It is said to give relief from the itching for several hours.
Fluocinonide gel .05 percent is another remedy I have heard helps with the extreme itching. Fortunately, I have not had an outbreak since I learned about this remedy.
Ever Onward
Though my doctor recommended the gluten free diet, he didn't tell me how to do it, and I found there was a lot to learn! Luckily, during that time in the midst of outbreaks, I was attending cooking school. The school was not gluten free, but I took all of the methods and lessons home and converted everything I learned to be allergy free. The diagnosis and certification from the school launched me on an epicurean adventure and changed the course of my life. I started the Alternative Cook to help others who want to eat safe, delicious foods.
If you are suffering with an incredibly itchy, pervasive rash, or know someone who is, consider that gluten could be the offender. Celiac disease is much more prevalent in this country than once thought. If you need moral support with DH, I'd love to hear from you.
Sources:
- Dahlbom, Ingrid, Korponay-Szabo, Ilma R, Kovacs, Judit B, Szalai, Zsuzsana, Maki, Markku, Hansson, Tony. "Prediction of Clinical and Mucosal Severity of Coeliac Disease and Dermatitis Herpetiformus by Quantification of IgA/IgG Serum Antibodies to Tissue Transglutaminase." Journal of Pediatric Gastroenterology and Nutrition. Vol. 50(2), February 2010, P 140-146.
- "Biologists ID Defense Mechanism of Leading Fungal Pathogen. Psych Central. June 25, 2004. psychcentral.com.
- Lee, John R., Hawkins, Virginia. What Your Doctor May Not Tell You About Menopause. Mass Market Paperback. September, 2004.







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now