
Celiac.com 04/15/2023 - Celiac disease is a chronic autoimmune disorder that affects the small intestine, triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. One often overlooked consequence of untreated and undiagnosed celiac disease is the potential for nutrient deficiencies. Due to the damage caused to the lining of the small intestine, absorption of various essential nutrients may be impaired, leading to deficiencies that can have wide-ranging health effects. In this article, we will explore the connection between celiac disease and nutrient deficiencies, focusing on several key vitamins, minerals, and other essential nutrients.
The most common nutrient deficiencies associated with celiac disease that may lead to testing for the condition include iron, vitamin D, folate (vitamin B9), vitamin B12, calcium, zinc, and magnesium. Celiac disease can disrupt the absorption of these essential nutrients, potentially leading to anemia, bone health issues, and other health complications. After a celiac disease diagnosis it is important to do follow up testing for these nutrient deficiencies, as well as a follow-up endoscopies/biopsies to make sure that a patient's damaged villi are healing properly. Many of those with celiac disease will need to take vitamin and mineral supplements at the time of their diagnosis, and some will need to continue taking them for life. Note that having nutrient deficiencies alone would not be enough for a definitive diagnosis of celiac disease, and further testing is required to make a formal diagnosis.
Boron
Celiac.com Sponsor (A12):
Boron is a trace mineral that plays a role in bone health, brain function, and metabolism of certain nutrients. Deficiency in boron is rare, but it can lead to symptoms such as muscle weakness, joint pain, and impaired cognitive function. Untreated and undiagnosed celiac disease can cause malabsorption of boron due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation of boron may be needed for individuals with celiac disease, especially if they have prolonged untreated celiac disease or other risk factors for deficiency.
Calcium
Calcium is an essential mineral that is crucial for bone health, nerve function, and muscle contraction. Deficiency in calcium can lead to symptoms such as weakened bones, muscle cramps, and numbness and tingling in the extremities. Malabsorption of calcium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of osteoporosis and other bone-related complications in individuals with celiac disease. Measuring blood levels of calcium alone is not always an accurate indicator of calcium deficiency because the body will leach calcium from the bones to maintain normal blood levels of calcium. Therefore, bone density loss and other secondary indicators are often better diagnostic tools for detecting calcium deficiency. Calcium supplementation, along with a calcium-rich diet, may be necessary for individuals with celiac disease to maintain adequate calcium levels and support bone health.
Chloride
Chloride is an electrolyte that is involved in maintaining proper fluid balance, nerve function, and acid-base balance in the body. Deficiency in chloride is rare, but it can lead to symptoms such as muscle weakness, lethargy, and irregular heartbeat. Malabsorption of chloride can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can disrupt the body's fluid balance and electrolyte levels, further complicating the health of individuals with celiac disease. Proper monitoring of chloride levels and supplementation may be necessary for individuals with celiac disease, especially if they have prolonged untreated celiac disease or other risk factors for deficiency.
Choline
Choline is an essential nutrient that plays a role in brain development, nerve function, and liver health. Deficiency in choline can lead to symptoms such as cognitive decline, liver dysfunction, and muscle damage. In celiac disease, malabsorption of choline can occur due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation of choline may be necessary for individuals with celiac disease, especially if they have prolonged untreated celiac disease or other risk factors for deficiency.
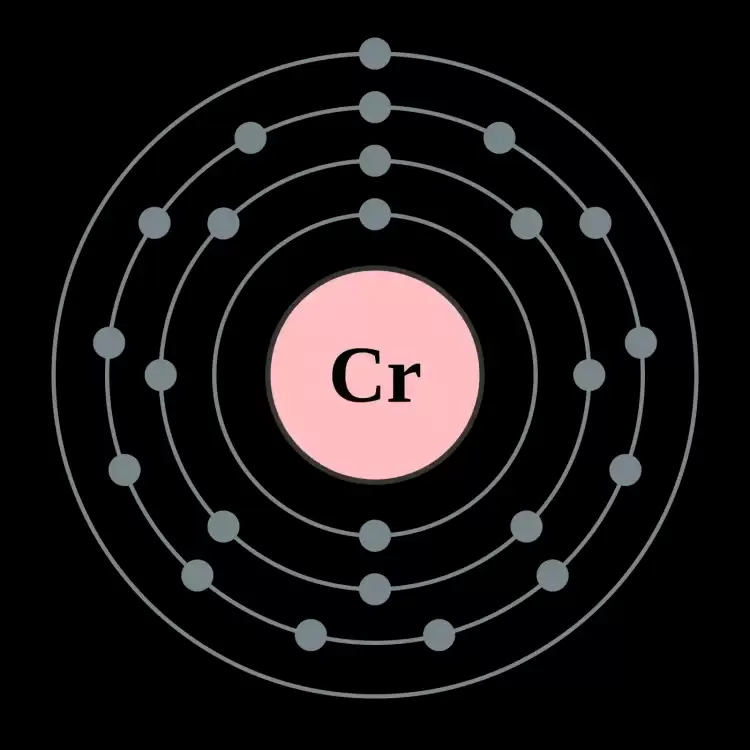
Image: CC BY-SA 2.0--User: Pumbaa (original work by commons:User: Greg Robson
Chromium
Chromium is a trace mineral that is important for glucose metabolism and insulin function. Deficiency in chromium can lead to symptoms such as impaired glucose tolerance, increased insulin resistance, and poor blood sugar control. Malabsorption of chromium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation of chromium may be needed for individuals with celiac disease, especially if they have poor blood sugar control or other risk factors for deficiency.
Copper
Copper is an essential trace mineral that plays a role in various processes in the body, including energy production, connective tissue formation, and immune function. Deficiency in copper can cause symptoms such as anemia, bone abnormalities, and impaired immune function. In celiac disease, malabsorption of copper can occur due to damage to the small intestine lining, potentially leading to a deficiency. This can further compromise the overall health of individuals with celiac disease and increase the risk of related complications. Supplementation of copper may be necessary for individuals with celiac disease to maintain adequate copper levels and support overall health.
Iodine
Iodine is a trace mineral that is essential for thyroid function, metabolism, and brain development. Deficiency in iodine can cause symptoms such as goiter, fatigue, weight gain, and impaired cognitive function. Malabsorption of iodine can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further disrupt thyroid function and metabolism, and impair cognitive development in individuals with celiac disease, especially in children. Iodine supplementation, along with a well-balanced diet that includes iodine-rich foods such as seafood and iodized salt, may be necessary for individuals with celiac disease to maintain adequate iodine levels and support overall health.
Iron
Iron is an essential mineral that is required for the production of hemoglobin, the protein in red blood cells that carries oxygen to all parts of the body. Deficiency in iron can cause symptoms such as anemia, fatigue, weakness, and pale skin. Malabsorption of iron can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further exacerbate the risk of anemia and related health issues in individuals with celiac disease. Iron supplementation, along with a well-balanced diet that includes iron-rich foods such as meat, poultry, beans, and fortified cereals, may be necessary for individuals with celiac disease to maintain adequate iron levels and support overall health.
Lutein
Lutein is a carotenoid antioxidant that is important for eye health and vision. Deficiency in lutein can cause symptoms such as blurred vision, macular degeneration, and increased risk of eye-related disorders. Malabsorption of lutein can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of eye-related issues and compromised vision in individuals with celiac disease. Lutein supplementation, along with a diet rich in lutein-containing foods such as leafy green vegetables, egg yolks, and corn, may be necessary for individuals with celiac disease to maintain adequate lutein levels and support overall eye health.
Lycopene
Lycopene is a carotenoid antioxidant that is known for its role in prostate health and reducing the risk of certain cancers. Deficiency in lycopene can cause symptoms such as increased risk of prostate cancer, cardiovascular disease, and oxidative stress. Malabsorption of lycopene can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of prostate cancer, cardiovascular issues, and other health complications in individuals with celiac disease. Lycopene supplementation, along with a diet rich in lycopene-containing foods such as tomatoes, watermelon, and red bell peppers, may be necessary for individuals with celiac disease to maintain adequate lycopene levels and support overall health.
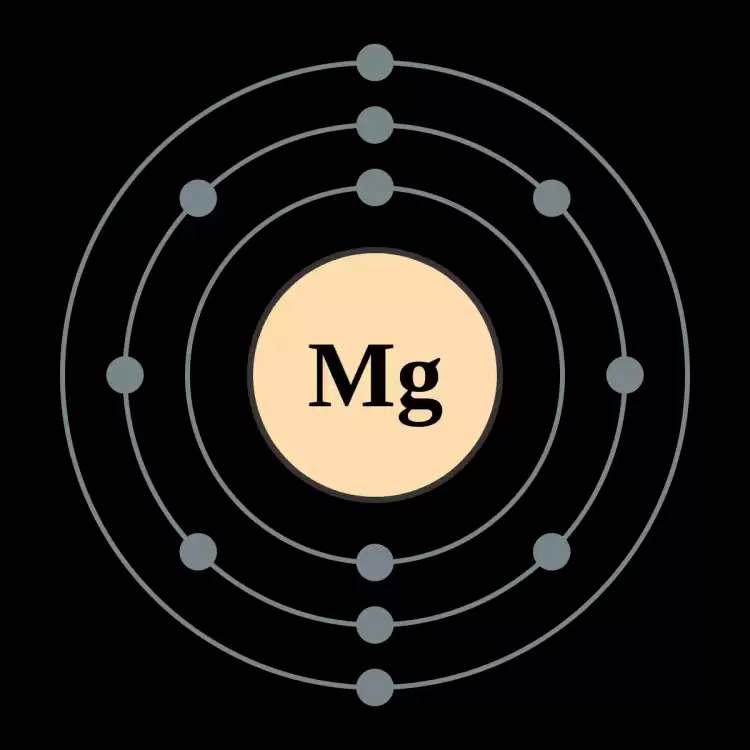
Image: CC BY-SA 2.0--User: Pumbaa (original work by commons: User: Greg Robson)
Magnesium
Magnesium is a vital mineral that plays a critical role in numerous physiological processes, including nerve function, muscle contraction, and bone health. Deficiency in magnesium can cause symptoms such as muscle weakness, tremors, irregular heartbeat, and bone loss. Malabsorption of magnesium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of muscle weakness, nerve-related issues, and compromised bone health in individuals with celiac disease. Magnesium supplementation, along with a diet rich in magnesium-containing foods such as leafy green vegetables, nuts, seeds, and whole grains, may be necessary for individuals with celiac disease to maintain adequate magnesium levels and support overall health.
Manganese
Manganese is an essential trace mineral that is involved in various metabolic processes, including carbohydrate metabolism and bone formation. Deficiency in manganese can cause symptoms such as impaired glucose tolerance, bone abnormalities, and altered cholesterol levels. Malabsorption of manganese can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of metabolic issues, bone-related complications, and altered cholesterol levels in individuals with celiac disease. Manganese supplementation, along with a diet rich in manganese-containing foods such as whole grains, nuts, seeds, and legumes, may be necessary for individuals with celiac disease to maintain adequate manganese levels and support overall health.
Molybdenum
Molybdenum is a trace mineral that is essential for various enzymatic reactions in the body, including detoxification processes and metabolism of certain nutrients. Deficiency in molybdenum is rare but can cause symptoms such as rapid heartbeat, neurological issues, and growth retardation. Malabsorption of molybdenum can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of cardiovascular issues, neurological complications, and growth retardation in individuals with celiac disease. Molybdenum supplementation, along with a diet rich in molybdenum-containing foods such as legumes, whole grains, and nuts, may be necessary for individuals with celiac disease to maintain adequate molybdenum levels and support overall health.
Nickel
Nickel is a trace mineral that is required in very small amounts for various enzymatic reactions in the body. Deficiency in nickel is rare and typically occurs in individuals with specific health conditions. Malabsorption of nickel can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of compromised enzymatic reactions and related health issues in individuals with celiac disease. Nickel supplementation is not typically necessary, as the body requires only trace amounts of nickel. However, it is important for individuals with celiac disease to maintain a well-balanced diet that includes nickel-containing foods such as nuts, legumes, and whole grains to support overall health.
Phosphorus
Phosphorus is an essential mineral that plays a crucial role in bone formation, energy metabolism, and cellular function. Deficiency in phosphorus is rare and usually occurs in individuals with specific health conditions or imbalanced diets. Malabsorption of phosphorus can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of compromised bone health, energy metabolism, and cellular function in individuals with celiac disease. Phosphorus supplementation is not typically necessary, as phosphorus is abundant in many foods. However, it is important for individuals with celiac disease to maintain a well-balanced diet that includes phosphorus-containing foods such as dairy products, meat, fish, nuts, seeds, and whole grains to support overall health.
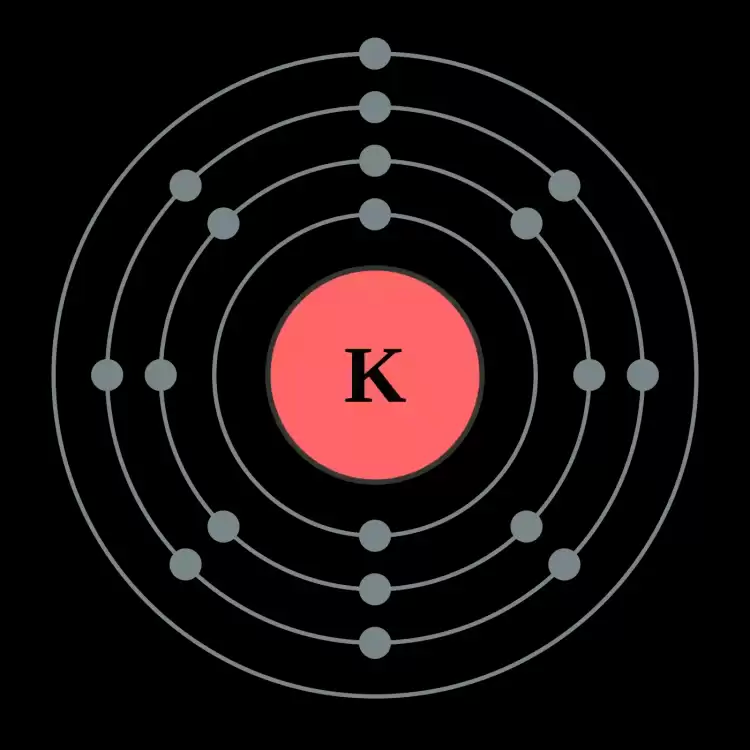
Image: CC BY-SA 2.0--User: Pumbaa (original work by commons: User: Greg Robson)
Potassium
Potassium is a crucial mineral that is involved in numerous physiological processes, including nerve function, muscle contraction, and heart health. Deficiency in potassium can cause symptoms such as muscle weakness, fatigue, irregular heartbeat, and increased blood pressure. Malabsorption of potassium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of nerve-related issues, muscle weakness, and cardiovascular complications in individuals with celiac disease. Potassium supplementation, along with a diet rich in potassium-containing foods such as fruits, vegetables, dairy products, meat, and legumes, may be necessary for individuals with celiac disease to maintain adequate potassium levels and support overall health.
Selenium
Selenium is an essential trace mineral that is involved in various antioxidant and immune functions in the body. Deficiency in selenium can cause symptoms such as compromised immune function, muscle weakness, fatigue, and hair loss. Malabsorption of selenium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of impaired immune function, muscle weakness, and related health issues in individuals with celiac disease. Selenium supplementation, along with a diet rich in selenium-containing foods such as fish, meat, dairy products, nuts, and seeds, may be necessary for individuals with celiac disease to maintain adequate selenium levels and support overall health.
Silicon
Silicon is a trace mineral that is involved in various processes such as bone formation, connective tissue health, and hair, skin, and nail health. Deficiency in silicon is rare, as it is found in many foods, but it can cause symptoms such as compromised bone health, weak connective tissue, and brittle nails. Malabsorption of silicon can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of compromised bone health, connective tissue issues, and related health concerns in individuals with celiac disease. Silicon supplementation is not typically necessary, as silicon is abundant in many foods. However, it is important for individuals with celiac disease to maintain a well-balanced diet that includes silicon-containing foods such as whole grains, fruits, vegetables, nuts, and seeds to support overall health and prevent deficiency.
Vanadium
Vanadium is a trace mineral that has been suggested to play a role in blood sugar regulation and bone health, although its exact functions are not yet fully understood. Vanadium deficiency is rare, as it is found in small amounts in many foods, and its requirement in the body is low. However, malabsorption of vanadium can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of compromised blood sugar regulation and bone health in individuals with celiac disease. Vanadium supplementation is not typically necessary, as the body's requirement for vanadium is minimal, and excessive intake can be toxic. However, it is important for individuals with celiac disease to maintain a well-balanced diet that includes foods rich in vanadium, such as seafood, mushrooms, whole grains, and vegetable oils, to support overall health.
Vitamin A (Preformed)
Vitamin A is a fat-soluble vitamin that plays a crucial role in vision, immune function, and cellular growth. Deficiency in vitamin A can lead to night blindness, dry skin, and increased susceptibility to infections. Untreated celiac disease can cause malabsorption of vitamin A due to damage to the small intestine lining, leading to a deficiency. It is important for individuals with celiac disease to monitor their vitamin A levels and consider supplementation if necessary.
Vitamin A (Betacarotenes)
Vitamin A in the form of betacarotenes is a precursor that is converted to vitamin A in the body as needed. Betacarotenes are found in colorful fruits and vegetables, and they play a role in maintaining healthy skin, vision, and immune function. Deficiency in betacarotenes can result in similar symptoms as vitamin A deficiency, including impaired vision and weakened immune system. In celiac disease, impaired absorption of betacarotenes can occur due to damage to the small intestine lining, leading to a potential deficiency.
Vitamin B1 (Thiamine)
Vitamin B1, also known as thiamine, is a water-soluble vitamin that is essential for energy metabolism, nerve function, and brain health. Deficiency in thiamine can cause symptoms such as muscle weakness, fatigue, and mental confusion. Severe, prolonged thiamine deficiency can result in beriberi, and symptoms include loss of sensation in extremities, symptoms of heart failure, swelling of the hands and feet, chest pain, feelings of vertigo, double vision, and memory loss. Untreated celiac disease can impair thiamine absorption due to damage to the small intestine lining, potentially leading to a deficiency. It is important for individuals with celiac disease to monitor their thiamine levels and consider supplementation if needed.
Vitamin B2 (Riboflavin)
Vitamin B2, also known as riboflavin, is another water-soluble vitamin that plays a key role in energy production, growth, and red blood cell formation. Deficiency in riboflavin can lead to symptoms such as cracked lips, sore throat, and skin rash. Celiac disease can cause impaired absorption of riboflavin due to damage to the small intestine lining, leading to a potential deficiency. Supplementation may be necessary for individuals with celiac disease to maintain adequate riboflavin levels.
Vitamin B3 (Niacin)
Vitamin B3, also known as niacin, is essential for energy metabolism, nervous system function, and DNA repair. Deficiency in niacin can result in a condition known as pellagra, characterized by symptoms such as diarrhea, dermatitis, and mental confusion. Malabsorption of niacin can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. It is important for individuals with celiac disease to monitor their niacin levels and consider supplementation if necessary.
Vitamin B5 (Pantothenic Acid)
Vitamin B5, also known as pantothenic acid, is involved in energy production, hormone synthesis, and nerve function. Deficiency in pantothenic acid can lead to symptoms such as fatigue, numbness and tingling in the hands and feet, and difficulty in coordination. In celiac disease, malabsorption of pantothenic acid can occur due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation may be necessary for individuals with celiac disease to maintain adequate pantothenic acid levels.
Vitamin B6
Vitamin B6, also known as pyridoxine, is a water-soluble vitamin that is important for brain development, immune function, and protein metabolism. Deficiency in vitamin B6 can cause symptoms such as depression, irritability, and weakened immune system. Untreated celiac disease can impair the absorption of vitamin B6 due to damage to the small intestine lining, potentially leading to a deficiency. It is important for individuals with celiac disease to monitor their vitamin B6 levels and consider supplementation if needed.
Vitamin B7 (Biotin)
Vitamin B7, also known as biotin, is essential for healthy skin, hair, and nails, as well as for metabolism of carbohydrates, fats, and proteins. Deficiency in biotin can result in symptoms such as hair loss, brittle nails, and skin rash. Malabsorption of biotin can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation may be necessary for individuals with celiac disease to maintain adequate biotin levels.
Vitamin B8 (Inositol)
Vitamin B8, also known as inositol, is involved in cell signaling, nerve function, and brain health. Deficiency in inositol can lead to symptoms such as mood swings, anxiety, and difficulty in concentration. In celiac disease, impaired absorption of inositol can occur due to damage to the small intestine lining, potentially leading to a deficiency. It is important for individuals with celiac disease to monitor their inositol levels and consider supplementation if necessary.
Vitamin B9 (Folate)
Vitamin B9, also known as folate, is important for DNA synthesis, red blood cell formation, and fetal development during pregnancy. Deficiency in folate can result in symptoms such as anemia, fatigue, and neural tube defects in newborns. Malabsorption of folate can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation of folate may be necessary for individuals with celiac disease, especially during pregnancy.
Vitamin B9 (Folic Acid)
Folic acid is the synthetic form of folate, often used in dietary supplements and fortified foods. It is converted to folate in the body and plays similar roles in DNA synthesis, red blood cell formation, and fetal development during pregnancy. Deficiency in folic acid can lead to the same symptoms as folate deficiency, including anemia and neural tube defects in newborns. Malabsorption of folic acid can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. It is important for individuals with celiac disease to monitor their folic acid levels and consider supplementation if needed.
Vitamin B12 ( Cobalamin)
Vitamin B12, also known as cobalamin, is essential for nerve function, DNA synthesis, and red blood cell formation. Deficiency in vitamin B12 can cause symptoms such as fatigue, weakness, and numbness and tingling in the hands and feet. In celiac disease, malabsorption of vitamin B12 can occur due to damage to the small intestine lining, potentially leading to a deficiency. This can further exacerbate the symptoms of celiac disease and affect overall health. Supplementation of vitamin B12 may be necessary for individuals with celiac disease to maintain adequate levels and prevent deficiency-related complications.
Vitamin C (Ascorbic Acid)
Vitamin C, also known as ascorbic acid, is a powerful antioxidant that plays a critical role in immune function, collagen synthesis, and wound healing. Deficiency in vitamin C can cause symptoms such as fatigue, weakened immune system, and slow wound healing. A severe vitamin C deficiency can also result in scurvy, and early symptoms of scurvy include weakness, feeling tired and having sore arms and legs. In celiac disease, malabsorption of vitamin C can occur due to damage to the small intestine lining, potentially leading to a deficiency. Supplementation of vitamin C may be necessary for individuals with celiac disease to maintain adequate levels and support immune function.
Vitamin D3
Vitamin D3, also known as the "sunshine vitamin," is crucial for bone health, immune function, and mood regulation. Deficiency in vitamin D3 can cause symptoms such as bone pain, muscle weakness, and increased susceptibility to infections. Malabsorption of vitamin D3 is common in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of osteoporosis, weakened immune system, and mood disorders in individuals with celiac disease. Vitamin D3 supplementation, along with adequate sunlight exposure and a vitamin D-rich diet, may be necessary for individuals with celiac disease to maintain adequate vitamin D levels and support overall health.
Vitamin E (Food Sourced)
Vitamin E is a powerful antioxidant that protects cells from damage, supports immune function, and helps with DNA repair. Deficiency in vitamin E can cause symptoms such as muscle weakness, impaired vision, and increased oxidative stress. Malabsorption of vitamin E can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of oxidative stress and related health issues in individuals with celiac disease. Vitamin E supplementation, along with a vitamin E-rich diet, may be necessary for individuals with celiac disease to maintain adequate vitamin E levels and support overall health.
Vitamin E (Alpha-Tocopherol)
Vitamin E, specifically alpha-tocopherol, is the most active and common form of vitamin E in the body. It plays a crucial role in protecting cells from damage, supporting immune function, and maintaining cardiovascular health. Deficiency in alpha-tocopherol can cause symptoms such as muscle weakness, vision problems, and increased risk of cardiovascular disease. Malabsorption of alpha-tocopherol can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of cardiovascular issues and other health complications in individuals with celiac disease. Supplementation of alpha-tocopherol, along with a vitamin E-rich diet, may be necessary for individuals with celiac disease to maintain adequate alpha-tocopherol levels and support overall health.
Vitamin K
Vitamin K is a fat-soluble vitamin that plays a crucial role in blood clotting and bone metabolism. Deficiency in vitamin K can cause symptoms such as easy bruising, prolonged bleeding, and weakened bones. Malabsorption of vitamin K can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of bleeding disorders and weakened bones in individuals with celiac disease. Vitamin K supplementation, along with a well-balanced diet that includes vitamin K-rich foods such as leafy green vegetables, may be necessary for individuals with celiac disease to maintain adequate vitamin K levels and support overall health.
Zinc
Zinc is an essential mineral that is involved in various enzymatic reactions, immune function, and wound healing. Deficiency in zinc can cause symptoms such as impaired immune function, delayed wound healing, hair loss, and skin issues. Malabsorption of zinc can occur in celiac disease due to damage to the small intestine lining, potentially leading to a deficiency. This can further increase the risk of compromised immune function, delayed wound healing, and related health issues in individuals with celiac disease. Zinc supplementation, along with a diet rich in zinc-containing foods such as meat, fish, dairy products, nuts, and seeds, may be necessary for individuals with celiac disease to maintain adequate zinc levels and support overall health.
Conclusion
In conclusion, untreated and undiagnosed celiac disease can lead to deficiencies in various nutrients due to malabsorption caused by damage to the small intestine lining. These deficiencies can result in a wide range of symptoms and health effects, including compromised bone health, impaired immune function, nerve-related issues, skin, hair, and nail problems, and other related health concerns. Therefore, it is crucial for individuals with celiac disease to be vigilant about their nutrient intake and work with healthcare professionals to ensure proper monitoring and management of their nutrient levels through a well-balanced diet and, if necessary, appropriate supplementation. Proper management of celiac disease, including adherence to a gluten-free diet, regular monitoring of nutrient levels, and appropriate supplementation when needed, can help individuals with celiac disease maintain optimal health and prevent nutrient deficiencies.
Vitamins and Minerals Generally Safe in Excess of Recommended Daily Allowance (RDA):
- Vitamin C (Ascorbic Acid): Excess vitamin C is usually excreted in the urine and is considered safe in higher doses. However, very high doses may cause digestive upset in some individuals.
- Vitamin B1 (Thiamine): Water-soluble, excess thiamine is generally excreted through urine. It is considered safe in higher doses but consult with a healthcare professional.
- Vitamin B2 (Riboflavin): Water-soluble, excess riboflavin is excreted in the urine and is generally safe in higher doses.
- Vitamin B3 (Niacin): Water-soluble, niacin has a well-defined upper limit, but moderate excess is often excreted. Consultation with a healthcare professional is advisable.
- Vitamin B5 (Pantothenic Acid): Water-soluble, excess pantothenic acid is generally excreted through urine and considered safe in higher doses.
- Vitamin B6 (Pyridoxine): While excessive intake from supplements can lead to nerve damage, moderate overages are generally excreted through urine.
- Vitamin B7 (Biotin): Water-soluble, excess biotin is typically excreted and is considered safe in higher doses.
- Vitamin B9 (Folate): Excess folate is usually excreted, but extremely high levels from supplements may have potential risks. It's generally safe when consumed through natural food sources.
- Vitamin B12 (Cobalamin): Water-soluble, excess B12 is typically excreted in the urine and is considered safe in higher doses. Consultation with a healthcare professional is advisable.
- Choline: While not a true vitamin, choline is water-soluble, and excess is usually excreted. It's considered safe in higher doses but consult with a healthcare professional.
Vitamins and Minerals with Potential for Toxicity in Excess of Recommended Daily Allowance (RDA):
- Vitamin A (Retinol): Excessive vitamin A intake, especially from supplements, can lead to toxicity, causing symptoms like nausea, dizziness, and, in severe cases, organ damage.
- Vitamin D - While moderate excess may be excreted, prolonged high doses can lead to vitamin D toxicity, resulting in hypercalcemia, kidney damage, and other complications.
- Vitamin E (Tocopherols): Excess vitamin E is usually excreted, but high doses from supplements may have adverse effects. Obtaining it through a balanced diet is preferable.
- Vitamin K: Excess vitamin K from supplements can interfere with blood thinning medications and cause issues in some individuals.
- Iron: Excessive iron intake, especially from supplements, can lead to iron toxicity, causing symptoms like nausea, abdominal pain, and, in severe cases, organ failure.
- Zinc: While zinc is essential, excessive intake can lead to zinc toxicity, affecting the immune system and causing digestive issues.
- Copper: High copper levels, often from supplements, can lead to toxicity, causing symptoms such as nausea, vomiting, and liver damage.
- Selenium: Excessive selenium intake, especially from supplements, can lead to selenosis, causing symptoms like hair loss, gastrointestinal issues, and neurological problems.
It's crucial to note that individual tolerances can vary, and supplementation should be done under the guidance of a healthcare professional.
Sources:
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Celiac Disease. Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease
- Rubio-Tapia, A., Hill, I. D., Kelly, C. P., Calderwood, A. H., & Murray, J. A. (2013). ACG clinical guidelines: Diagnosis and management of celiac disease. The American Journal of Gastroenterology, 108(5), 656-676. doi:10.1038/ajg.2013.79
- Complementary Medicine, Penn State Hershey. (n.d.). B vitamins. Retrieved from https://pennstatehershey.adam.com/content.aspx?productId=107&pid=33&gid=000336
- National Institutes of Health, Office of Dietary Supplements. (2021). Vitamin B5 (Pantothenic Acid) - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Vitamin B12 - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Chloride - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Iodine - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Magnesium - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Phosphorus - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Silicon - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Vanadium - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Manganese - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Lycopene - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Lutein and Zeaxanthin - Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Nickel - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Selenium - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Iron - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Calcium - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Zinc - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/
- National Institutes of Health, Office of Dietary Supplements. (2021). Chromium - Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/list-all/







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now