
Celiac.com 11/10/2016 - So far, 2014 has been a challenging new year for me. I was reminded of some events that happened almost fifty years ago. Based on that reminder, I resolved to contact a former girlfriend, both to suggest that she get testing for celiac disease, and to apologize for some insensitive things I said and did when I was 17. She was a year younger than me and one grade behind me in school. She was very slender and exceedingly self-conscious about having what she called "a chest like a boy". (She may have been experiencing delayed development, as is sometimes seen in celiac disease.) Every new place we visited, she went looking for the washroom as soon as she could. Movie theatres, restaurants, libraries, everywhere we went, she found the washroom first. She even did that the first time she was at my mother's house, which occasioned an uncharitable comment from my mom.
Pat was also troubled by some microscopic hair that was growing on her upper lip. It sounds silly now, but these things were important to her at the time. I remember telling her that nobody could see her "moustache" without a magnifying glass. Nonetheless, she put Nair on it and, for at least one day, had the brightest red upper lip I have ever seen. She said it was too sore to put makeup on, so it really drew a lot of unwanted attention. Until meeting my wife, I never knew anyone who was as honest about who she was. I regret that I didn't appreciate her as much as I should have, but that was partly due to my age.
Celiac.com Sponsor (A12):
Time passed, way led onto way, and life happened. Forty nine years later, there I was, looking for her on Facebook and other social media. I tracked her through old phone numbers, family members, and I even searched the title on her parents' home. I was full of excitement about re-connecting with my old friend, a person with whom I had shared those last innocent days of adolescence. Our friendship had been cut short because her dad was transferred to a city more than 600 miles away, and she was annoyed with me because I had said and done some insensitive things. We never even wrote to each other. I used to talk about her with my students, explaining our mutual fascination with literature. I thought about her often, but never, until this year, considered contacting her.
After about a month of searching, I eventually found her. Much to my dismay, I was almost a year too late. She had passed away on March 10th of 2013, at the age of 64. At the time of her death, she was in the process of being evaluated for Parkinson's disease. She was at home when she experienced her last, massive seizure, which resulted in brain death. Both of her daughters are heartbroken over Pat's sudden, unexpected passing. Already a widow, Pat had left this world before I took the time and made the effort to be in touch with her again. I was filled with sadness, disappointment, and regret when I first reached one of her daughters and confirmed that she was the person I had known. I still wonder, if I had gotten in touch a decade earlier, would she still be alive? Would a gluten-free diet have helped her? I'll never know, but the relevant literature does seem to suggest that a gluten-free diet may have helped (1, 2).
Then, a week or so ago, I received an email from a concerned mom. Her athletic, teen-aged son was recovering from a brain concussion he had sustained. His friends who had sustained similar concussions, at other times, reported having recovered more quickly. His mom began to wonder if her son's slow recovery could be the result of his celiac disease, despite more than a decade of strict compliance with the diet. I didn't know. I could only offer the suggestions that he try daily supplementation with medium chain triglycerides, and a ketogenic diet, as they seem to have stopped my life-long tremors. I also suggested that he try avoiding dairy and soy as well, based on research I did 14 years ago for my grandson.
This concerned mom also mentioned, "I generally find doctors are dismissive of the idea that celiac is linked to any issues outside the digestive tract, unless it's malnutrition-related, and they tend to think everything should be hunky-dory if you just follow the gluten-free diet." She went on to say that "It gets kind of old being thought of as the silly, overprotective mom."
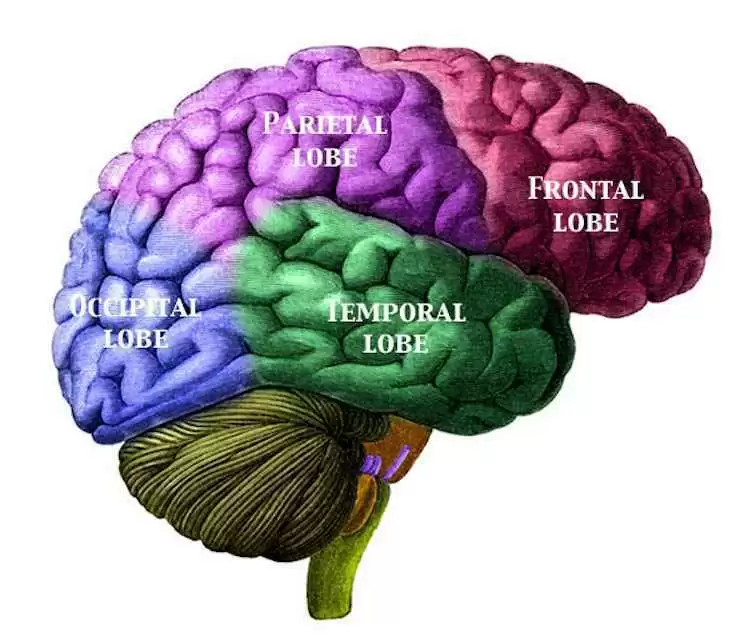
Neurological researchers have long known about a correlation between a variety of neurological ailments and gluten sensitivity, with or without celiac disease (3). We also know that neurological symptoms are commonly found among more than half of patients with celiac disease (4). Also, despite modern diagnostic protocols and technology, we are still seeing some overlap between celiac disease and both amyotrophic lateral sclerosis (5) and multiple sclerosis (6) as well as other neurological illnesses. For instance, the increased presence of the gene named Parkinson's disease 7 (PARK7) has been found in the duodenal mucosa of untreated children with celiac disease and may be implicated in the alteration of the permeability of their intestinal barriers (7). This further suggests an important link between gluten sensitivity and Parkinson's disease. This gene may predispose to the appearance of this most distressing disease later in life.
Many people with celiac disease continue to experience neurological symptoms, despite compliance with a gluten-free diet. This may suggest that the neurodegenerative dynamics, once initiated by gluten ingestion, may continue, either in the absence of gluten or in response to trace amounts of gluten (10). I also started to wonder if the cellular and immune system clean-up processes that follow brain injuries might initiate some of the same damaging autoimmune processes in the brain? They might also occur in response to other dietary factors which may trigger autoimmune dynamics that mimic reactions to gluten, or maybe there is some other, unknown factor that triggers the brain damage.
One research group on the leading edge of the investigation of gluten sensitivity in relation to neurological illnesses reports that, "Incomplete elimination of gluten from the diet may be enough to abolish gastrointestinal symptoms with recovery of the small bowel mucosa but is insufficient to arrest the state of heightened immunological responsiveness resulting in neuronal injury" (10). So, when it comes to even tiny amounts of gluten, they may be enough to perpetuate gluten induced neurological illnesses. There may also an agent in the environment that is causing a cross reaction. This area really needs more investigation, as baby boomers threaten alarmingly increased rates of all forms of dementia.
We already know that people with celiac disease are at much greater risk of developing neurological diseases than the general population (13). These ailments range from headaches to learning disabilities to movement disorders to tic disorders, to seizures, to sensory disorders (4) and many who have non-celiac gluten sensitivity also experience a high rate of neurological disease (3). Does that also mean that young athletes with celiac disease will take longer to recover from head injuries?
Does it also mean, given the slow acceptance of gluten as a factor in many common neurological illnesses (11) that people like my former high school flame will never be told about the neuro-protective benefits of a gluten-free diet or a ketogenic diet? Surely, resistance to the well established data showing neurological manifestations of gluten sensitivity as a scientific fact (12) is more emotional than rational. A gluten-free diet and/or a ketogenic diet should be offered to those people regardless of whether their neurologist is either resistant to, or not staying current with, his/her professional literature. But they cannot offer what they do not know or have developed some bias against. Dr. David Perlmutter has done an excellent job of getting the word out to the general public, with his recent book titled Grain Brain, but there is much more work to do.
People who are gluten sensitive, and are therefore at greater risk of developing neurological disease, might be well advised to look carefully at the benefits of a high fat, ketogenic diet, and the benefits of supplementing with medium chain triglycerides and Omega 3 fatty acids (14). Equally, they might be well advised to avoid the pro-inflammatory omega 6 and omega 9 fatty acids, as well as limiting the amounts of polyunsaturated fats they eat, which are also pro-inflammatory 14). I find that I feel my best when I am in mild, diet-induced ketosis (about 15 mg/dl as measured in morning urine, with Ketostix, which are inexpensive and available at most drug stores). There are a number of good books that explore the fine points of a high fat, ketogenic diet. These include The Art and Science of Low Carbohydrate Living by Volek and Phinney, The Ketogenic Diet by Lyle McDonald, and many others.
Finally, when considering a gluten-free diet for neurological ailments, it is important to recognize that 20 parts per million may be far too much gluten to consume. The maximum threshold to qualify as gluten-free under the United Nations Codex Alimentarius Commission and many other regulatory agencies, including the FDA, is 20 parts per million. Without further research, especially in the field of neurology and gluten sensitivity, we will never know what, if any, levels of gluten are safe to consume.
Regardless of the nature of your neurological ailment, whether it is Parkinson's disease, or seizures, or multiple sclerosis, or amyotrophic lateral sclerosis, or brain cancer, or almost any other kind of cancer (15), or even if you are just slow recovering from a neurological injury, the positive results of dietary interventions might offer you a whole new lease on life.
Sources:
- Open Original Shared Link
- Currie S, Hadjivassiliou M, Clark MJ, Sanders DS, Wilkinson ID, Griffiths PD, Hoggard N. Should we be ‘nervous' about coeliac disease? Brain abnormalities in patients with coeliac disease referred for neurological opinion. J Neurol Neurosurg Psychiatry. 2012 Dec;83(12):1216-21.
- Matheson NA. Letter: Food faddism. Am J Clin Nutr. 1975 Oct;28(10):1083.
- Zelnik N, Pacht A, Obeid R, Lerner A. Range of neurologic disorders in patients with celiac disease. Pediatrics. 2004 Jun;113(6):1672-6.
- Brown KJ, Jewells V, Herfarth H, Castillo M, White matter lesions suggestive of amyotrophic lateral sclerosis attributed to celiac disease. AJNR Am J Neuroradiol. 2010 May;31(5):880-1
- Batur-Caglayan HZ, Irkec C, Yildirim-Capraz I, Atalay-Akyurek N, Dumlu S. A case of multiple sclerosis and celiac disease. Case Rep Neurol Med. 2013;2013:576921.
- Vörös P, Sziksz E, Himer L, Onody A, Pap D, Frivolt K, Szebeni B, Lippai R, GyÅ‘rffy H, Fekete A, Brandt F, Molnár K, Veres G, Arató A, Tulassay T, Vannay A. Expression of PARK7 is increased in celiac disease. Virchows Arch. 2013 Sep;463(3):401-8.
- Hadjivassiliou M, Grünewald RA, Lawden M, Davies-Jones GA, Powell T, Smith CM. Headache and CNS white matter abnormalities associated with gluten sensitivity. Neurology. 2001 Feb 13;56(3):385-8.
- Hadjivassiliou M, Sanders DS, Grünewald RA, Woodroofe N, Boscolo S, Aeschlimann D. Gluten sensitivity: from gut to brain. Lancet Neurol. 2010 Mar;9(3):318-30
- Hadjivassiliou M, Grünewald RA, Davies-Jones GA. Gluten sensitivity as a neurological illness. J Neurol Neurosurg Psychiatry. 2002 May;72(5):560-3.
- Tengah P, AJ Wills. Questions and Answers About the Neurology of Gluten Sensitivity. Pract Neurol 2003;3:354-357
- Hadjivassiliou M, Grünewald R. The Neurology of Gluten Sensitivity: science Vs conviction. Pract Neurol 2004;3:4, 124-126.
- Hadjivassiliou M, Grünewald R. Gluten sensitivity as a neurological illness. Neurol Neurosurg Psychiatry. May 2002; 72(5): 560–563.
- Open Original Shared Link
- Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013 Aug;67(8):789-96






Recommended Comments