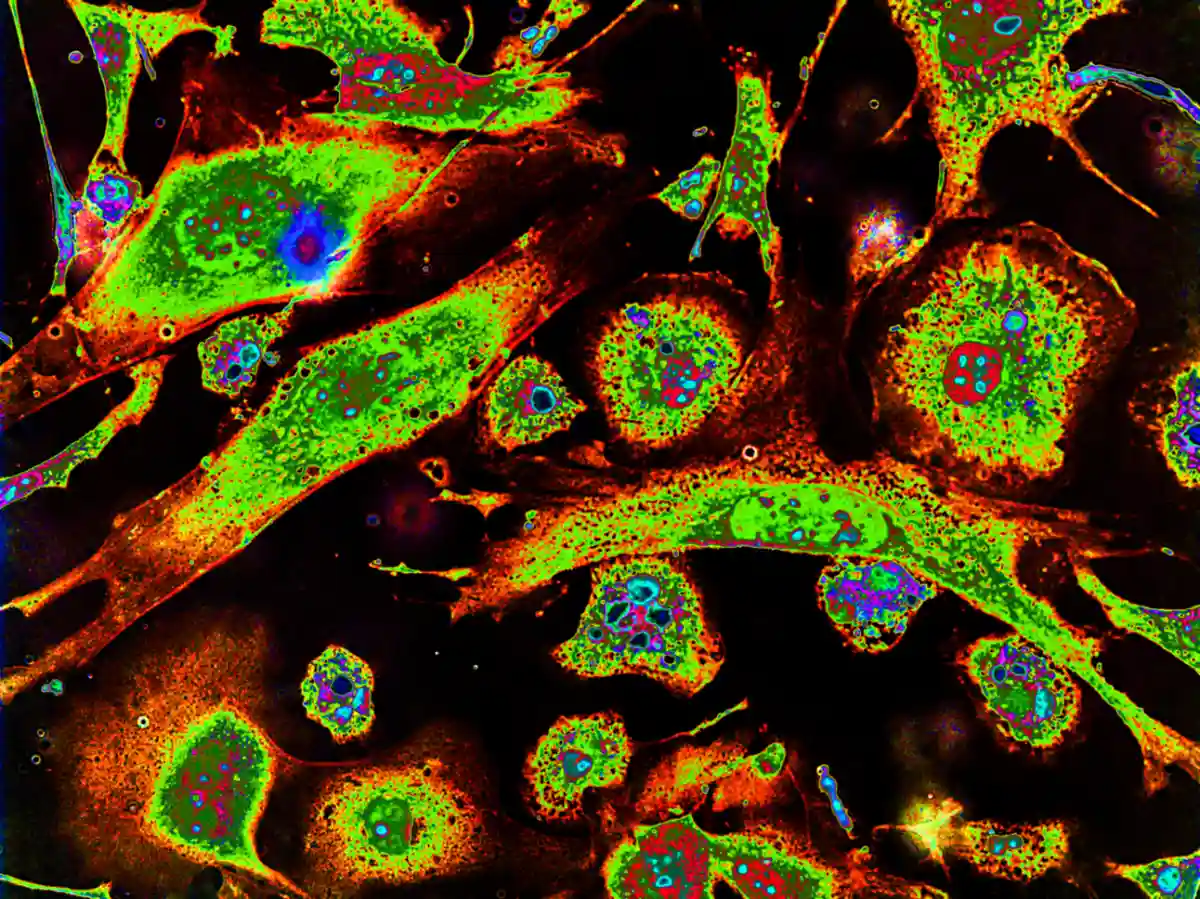
Celiac.com 07/03/2023 - Celiac disease is an autoimmune disorder caused by eating gluten, which damages the small intestine. We know that the immune system plays a crucial role in the development of the disease, which involves various types of immune cells.
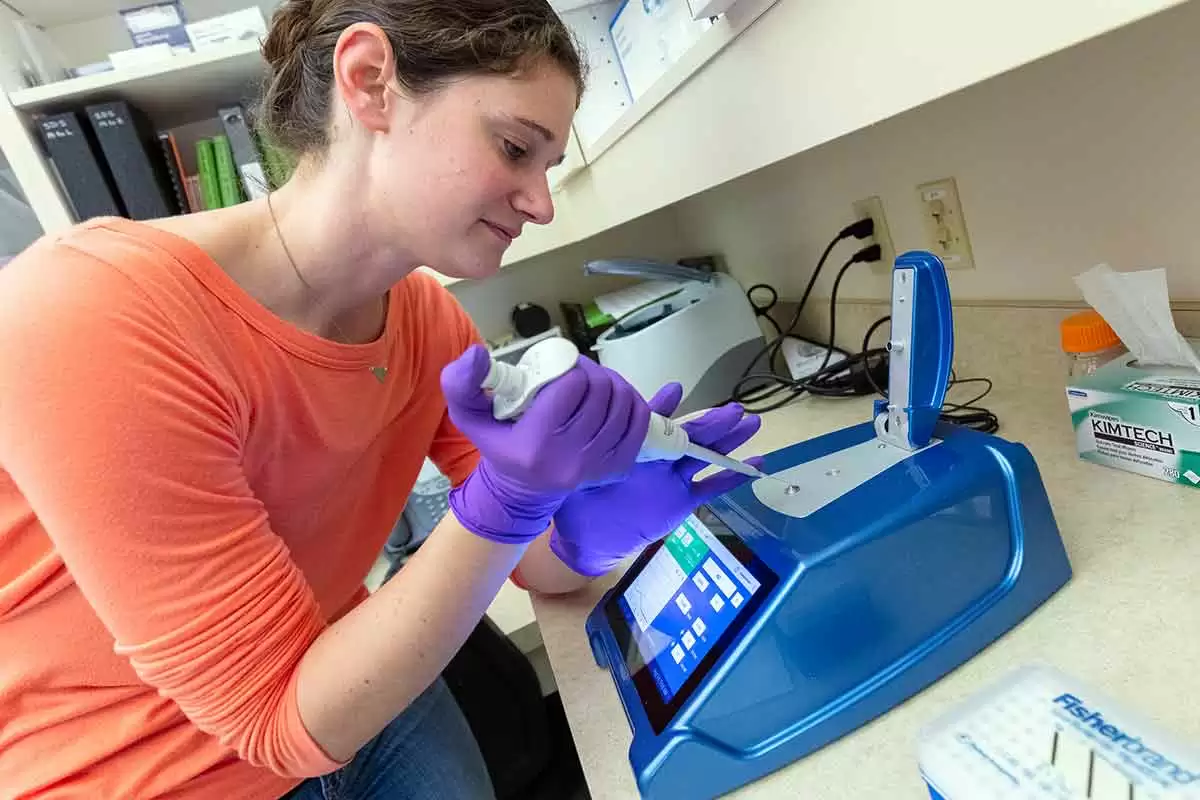
In a recent study, researchers Nader Atlasy, Anna Bujko of the Department of Molecular Biology, Faculty of Science, Radboud University, Nijmegen, The Netherlands, examined the immune cells in the small intestine of individuals with celiac disease to understand their role in the disease.
Macrophages are Reduced in Celiac Disease Patients Increasing Inflammation
Celiac.com Sponsor (A12):
Their study found that certain immune cells called macrophages were reduced in celiac disease. These cells showed changes in their gene activity in response to a signaling molecule called interferon-gamma (IFNg). This signaling pathway may contribute to the accumulation of pro-inflammatory macrophages in celiac disease. The study also observed differences in the gene activity of mast cells, which are involved in the immune response, between individuals with celiac disease and those following a gluten-free diet.
New Genetic Markers Identified May Trigger Celiac Disease
The number of CD3+ T cells, a type of immune cell, was increased in celiac disease. The gene activity of CD4+ and CD8+ T cells, subtypes of CD3+ T cells, was significantly different from healthy individuals and those on a gluten-free diet. These T cells expressed genes related to infections, suggesting a potential link between altered intestinal bacteria and celiac disease.
The study identified a population of CD4+ T cells with regulatory properties, indicated by the expression of TIGIT and IKZF2 (Helios). CD4+ T cells in celiac disease displayed a mixed phenotype of activated cells and cells with regulatory properties. CD8+ T cells in the gut also showed an activated gene activity pattern, suggesting their involvement in celiac disease.
Furthermore, the study identified a distinct population of intraepithelial lymphocytes (IELs) in the small intestine. This population was reduced in people with celiac disease, and only partially restored in individuals following a gluten-free diet. The decrease in this population may contribute to the development of celiac disease.
The findings also suggested a potential role of viral or bacterial stimuli in celiac disease, as certain pathways associated with viral and bacterial responses were upregulated in immune cells of individuals with the disease.
Read more in Nature Communications volume 13, Article number: 4920 (2022)


.webp.c53b640f544ac5b6827ea9b8bf621ae6.webp)





Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now