Celiac.com 02/28/2025 - Celiac disease, an autoimmune disorder triggered by the ingestion of gluten, is commonly associated with digestive issues such as bloating, diarrhea, and abdominal pain. However, its effects extend far beyond the gastrointestinal system. For many people with celiac disease or gluten sensitivity, the condition can manifest through a range of skin-related symptoms and disorders. Understanding the link between celiac disease and skin conditions is crucial for effective diagnosis and treatment.
This article will explore the key skin conditions associated with celiac disease, how gluten impacts skin health, and what people with celiac disease or gluten sensitivity can do to manage these issues.
Dermatitis Herpetiformis: The Skin's Gluten Alarm
Celiac.com Sponsor (A12):
One of the most well-known skin conditions directly linked to celiac disease is dermatitis herpetiformis. Often referred to as "the skin manifestation of celiac disease," this condition is characterized by intensely itchy, blistering skin rashes.
What Causes Dermatitis Herpetiformis?
When someone with celiac disease consumes gluten, their immune system reacts by producing antibodies. These antibodies can mistakenly target the skin, leading to the formation of itchy, red bumps and blisters. These rashes often appear symmetrically on areas like the elbows, knees, buttocks, and scalp.
Why Is Dermatitis Herpetiformis Significant?
Dermatitis herpetiformis is a strong indicator of celiac disease, even if the individual does not experience typical digestive symptoms. In fact, some people with dermatitis herpetiformis may have "silent" celiac disease, where the condition affects their body without causing noticeable gastrointestinal distress.
How Is It Treated?
The most effective treatment for dermatitis herpetiformis is adopting a strict gluten-free diet. Additionally, medications like dapsone can provide short-term relief from itching and inflammation while the diet takes effect.
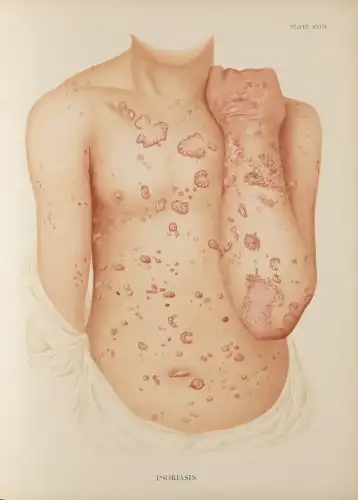
Psoriasis and Its Gluten Connection
Psoriasis, an autoimmune condition that causes the rapid buildup of skin cells leading to scaling and inflammation, is another skin disorder that may have ties to celiac disease.
The Immune System Overlap
Both psoriasis and celiac disease involve an overactive immune system. Research suggests that people with celiac disease may have a higher likelihood of developing psoriasis due to shared genetic and immunological pathways.
The Role of Gluten in Psoriasis Flares
For some individuals with psoriasis, gluten can exacerbate symptoms. Although not everyone with psoriasis has gluten sensitivity, removing gluten from the diet has been shown to improve skin health in those who test positive for gluten-related antibodies.
Managing Psoriasis with Celiac Disease
If you have both celiac disease and psoriasis, adhering to a gluten-free diet may help reduce inflammation and improve skin symptoms. Working with a healthcare provider to identify additional triggers, such as stress or certain foods, is also essential.
Eczema and Gluten Sensitivity
Eczema, or atopic dermatitis, is a chronic skin condition that causes dry, itchy, and inflamed patches of skin. While eczema is not directly caused by celiac disease, there is evidence to suggest a potential connection for some individuals.
How Gluten May Aggravate Eczema
In people with celiac disease or gluten sensitivity, consuming gluten can trigger systemic inflammation, which may worsen eczema symptoms. Additionally, nutrient deficiencies commonly associated with celiac disease, such as low levels of zinc and essential fatty acids, can impair skin barrier function and contribute to eczema flare-ups.
Dietary Changes for Eczema Relief
Eliminating gluten and ensuring adequate nutrition can play a significant role in managing eczema. Many individuals report improvements in their skin after adopting a gluten-free diet, though results may vary depending on other contributing factors like allergies or environmental triggers.
Gluten and General Skin Sensitivity
Beyond specific conditions like dermatitis herpetiformis, psoriasis, and eczema, gluten consumption may contribute to broader skin sensitivity and irritation in people with celiac disease or gluten intolerance.
Common Symptoms of Gluten-Related Skin Issues
- Persistent itching or rashes without a clear cause
- Dry or flaky skin despite using moisturizers
- Increased susceptibility to skin infections or delayed wound healing
These symptoms often arise due to immune system activation or nutrient deficiencies resulting from celiac disease.
The Importance of Nutrient Absorption for Skin Health
One of the less obvious ways celiac disease impacts the skin is through malabsorption of essential nutrients. The small intestine plays a vital role in absorbing vitamins and minerals, but damage caused by gluten in people with celiac disease can disrupt this process.
Key Nutrients for Skin Health
- Vitamin A: Essential for skin repair and reducing inflammation.
- Vitamin E: Protects skin cells from oxidative damage.
- Zinc: Supports wound healing and immune function.
- Omega-3 Fatty Acids: Help maintain skin hydration and reduce redness.
Addressing nutrient deficiencies through supplements or a nutrient-rich gluten-free diet can significantly improve skin health in individuals with celiac disease.
Diagnosing and Treating Skin Conditions in Celiac Disease
If you suspect that your skin issues are related to gluten or celiac disease, consulting a healthcare provider is crucial. Proper diagnosis often involves a combination of blood tests, skin biopsies, and, in the case of dermatitis herpetiformis, direct immunofluorescence testing.
Steps for Effective Treatment
- Adopt a Gluten-Free Diet: This is the cornerstone of managing both celiac disease and its related skin conditions.
- Address Nutritional Gaps: Work with a dietitian to ensure your gluten-free diet provides all necessary nutrients for optimal skin health.
- Topical Treatments: For conditions like eczema or psoriasis, use medicated creams or ointments to manage symptoms.
- Medications When Needed: In severe cases, medications like dapsone or biologics may be prescribed.
What This Means for People with Celiac Disease or Gluten Sensitivity
The link between celiac disease and skin conditions underscores the systemic nature of this autoimmune disorder. Recognizing skin issues as potential manifestations of celiac disease can lead to earlier diagnosis and more comprehensive management.
For those already diagnosed with celiac disease, understanding the connection to skin health emphasizes the importance of strict adherence to a gluten-free diet. Not only can this dietary change alleviate digestive symptoms, but it can also improve skin conditions, enhance overall quality of life, and reduce the risk of long-term complications.
By paying attention to their skin and seeking appropriate care, individuals with celiac disease or gluten sensitivity can take control of their health and achieve relief from both visible and hidden symptoms of gluten-related damage.
Conclusion
The relationship between celiac disease and skin conditions highlights the far-reaching impact of gluten on the body. From dermatitis herpetiformis to broader skin sensitivities, these issues can serve as important clues in diagnosing and managing celiac disease. By adopting a gluten-free diet and addressing associated nutrient deficiencies, individuals can take significant steps toward healthier skin and a better quality of life.
For anyone experiencing unexplained skin issues, especially when combined with gastrointestinal symptoms, exploring the possibility of celiac disease or gluten sensitivity may provide much-needed answers and relief.









Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now