Celiac.com 03/05/2025 - Celiac disease is a complex autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. While the condition is often discussed in terms of dietary management, its genetic underpinnings play a crucial role in determining who might develop the disease. Understanding the genetic basis of celiac disease can help individuals and their families assess their risk, take preventive measures, and seek timely diagnosis and treatment.
The Genetic Basis of Celiac Disease
Celiac disease is strongly associated with specific genetic markers found in the human leukocyte antigen (HLA) region of the immune system. The HLA-DQ2 and HLA-DQ8 genes are present in nearly all individuals diagnosed with celiac disease. These genes encode proteins that play a critical role in the immune response, particularly in recognizing and responding to gluten.
- HLA-DQ2: Found in approximately 90–95% of people with celiac disease.
- HLA-DQ8: Present in about 5–10% of individuals with the condition.
Celiac.com Sponsor (A12):
While the presence of these genes is a necessary factor for developing celiac disease, it is not sufficient on its own. About 30–40% of the general population carries one or both of these genetic markers, but only a small percentage—approximately 1%—will go on to develop the disease. This indicates that environmental factors, such as gluten exposure, infections, or other triggers, also play a role in disease onset.
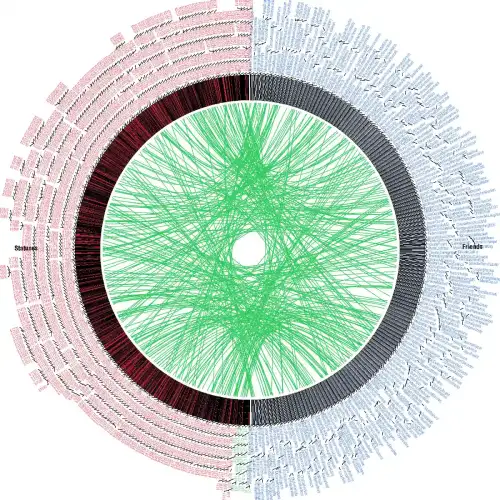
Understanding Family Risk
Celiac disease has a significant familial component, meaning that individuals with a family history of the condition are at a higher risk of developing it themselves. First-degree relatives—parents, siblings, or children—of someone with celiac disease have about a 10–15% chance of being diagnosed with the disorder. This is significantly higher than the 1% prevalence in the general population.
- First-degree relatives: As noted, these individuals face the highest risk.
- Second-degree relatives: Grandparents, aunts, uncles, and cousins also have a slightly increased risk compared to the general population, though not as high as first-degree relatives.
Given this heightened risk, family members of individuals with celiac disease are often advised to undergo genetic testing or screening, particularly if they exhibit symptoms or belong to another high-risk group.
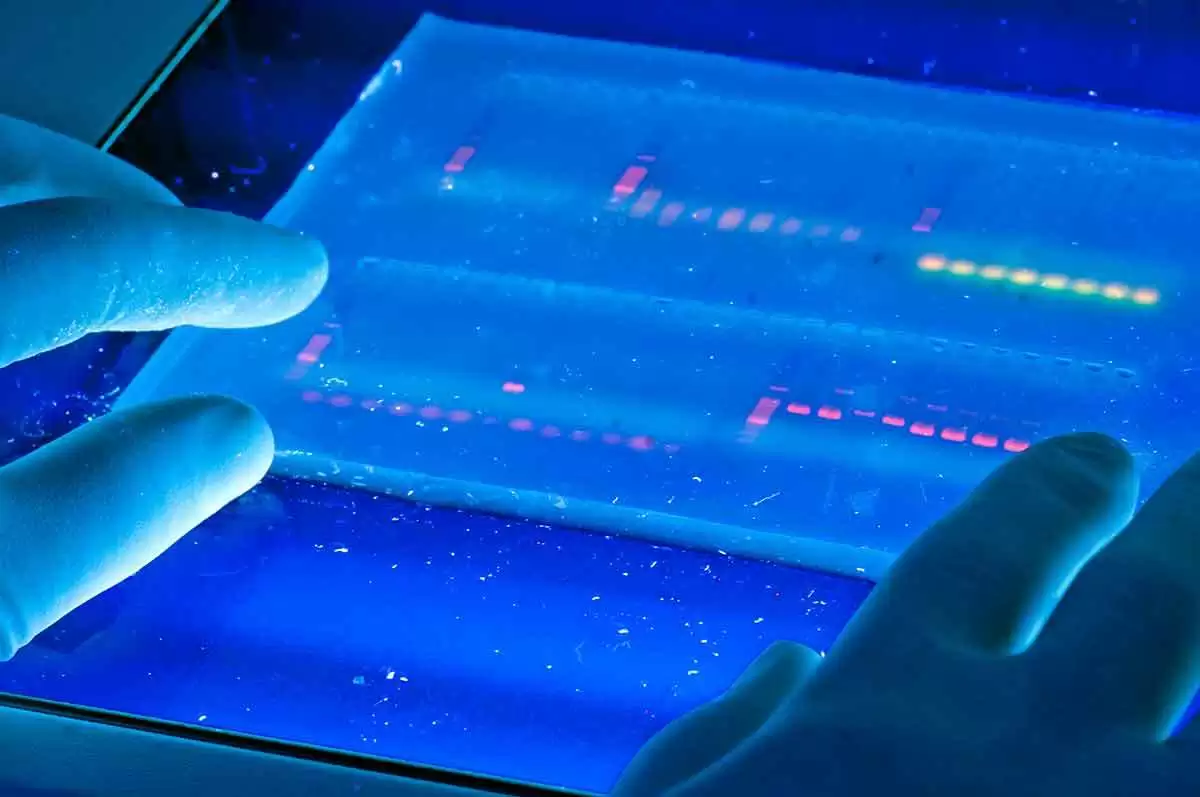
Genetic Testing: What It Can and Cannot Do
Genetic testing for celiac disease involves analyzing an individual’s DNA to determine if they carry the HLA-DQ2 or HLA-DQ8 genes. This test is particularly useful in the following scenarios:
Rule Out Celiac Disease: If a person does not carry either of these genes, they cannot develop celiac disease. This can be reassuring for family members concerned about their risk.
Risk Assessment: Identifying the presence of HLA-DQ2 or HLA-DQ8 can confirm a genetic predisposition, though it does not guarantee the person will develop the condition.
It's important to note that genetic testing cannot diagnose celiac disease. A positive genetic test only indicates susceptibility. For a definitive diagnosis, additional tests—such as blood tests for celiac-specific antibodies and intestinal biopsies—are required.
Environmental and Lifestyle Factors
Although genetics lay the foundation for celiac disease, environmental factors determine whether the condition will develop. Gluten consumption is the primary environmental trigger, but other factors, such as gut infections, microbiome imbalances, and stress, may influence disease onset.
Interestingly, some research suggests that the timing and amount of gluten introduced during infancy may impact the likelihood of developing celiac disease. However, there is no universally accepted guideline for preventing the disease through dietary measures in early childhood.
What Family Members Should Do
If you have a family member with celiac disease, here are steps to consider:
1. Consider Genetic Testing
Genetic testing can provide valuable information about your risk. If you do not carry the HLA-DQ2 or HLA-DQ8 genes, you can be fairly confident that the likelihood that you could develop celiac disease is very low. If you do carry one or both genes, you and your healthcare provider can monitor for symptoms and conduct periodic screening.
2. Stay Alert for Symptoms
Celiac disease can present with a wide range of symptoms, including digestive issues (diarrhea, bloating, and abdominal pain), fatigue, skin rashes, and even neurological symptoms. Some people may have no symptoms at all, a condition known as silent or asymptomatic celiac disease. Family members with unexplained health issues should discuss the possibility of celiac disease with their doctors.
3. Screen High-Risk Groups
In addition to family members, certain groups are at higher risk of celiac disease, including individuals with other autoimmune conditions like type 1 diabetes, thyroid disorders, or rheumatoid arthritis. Screening is particularly important for these groups.
4. Educate Yourself
Understanding the disease, its symptoms, and its potential complications can help you take proactive steps. If a diagnosis is made, transitioning to a gluten-free diet is essential for managing the condition and preventing long-term complications.
Why This Matters to Families
Celiac disease is more than just a dietary inconvenience; it is a serious autoimmune condition that can lead to complications if left untreated. Knowing your genetic risk can empower you to make informed decisions about your health. For families with a history of celiac disease, genetic testing and vigilant monitoring can lead to early detection, reducing the risk of complications like malnutrition, osteoporosis, and intestinal damage.
Additionally, understanding the genetic aspect of celiac disease can foster a sense of solidarity among family members. By supporting one another—whether through shared gluten-free meals or attending doctor’s appointments together—families can navigate the challenges of this condition more effectively.
Conclusion
The genetic basis of celiac disease underscores the importance of family history in assessing risk. While carrying the HLA-DQ2 or HLA-DQ8 genes does not guarantee a diagnosis, it does indicate susceptibility, making genetic testing a valuable tool for families. For those who test positive, regular monitoring and early intervention can make a significant difference in managing the disease. Ultimately, raising awareness about the genetic and familial aspects of celiac disease can help individuals and their loved ones live healthier, gluten-free lives.








Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now