Celiac.com 08/21/2024 - Celiac disease is an autoimmune disorder where the ingestion of gluten, a protein found in wheat, barley, and rye, leads to damage in the small intestine. The condition is marked by an immune response that targets and destroys the mucosal lining of the small intestine, causing symptoms such as bloating, diarrhea, constipation, nausea, and gas. The only effective treatment currently available is a lifelong adherence to a strict gluten-free diet. Traditional methods for studying celiac disease include the use of biopsied intestinal tissue, which has limitations in longevity and complexity, or animal models that do not fully replicate the human condition.
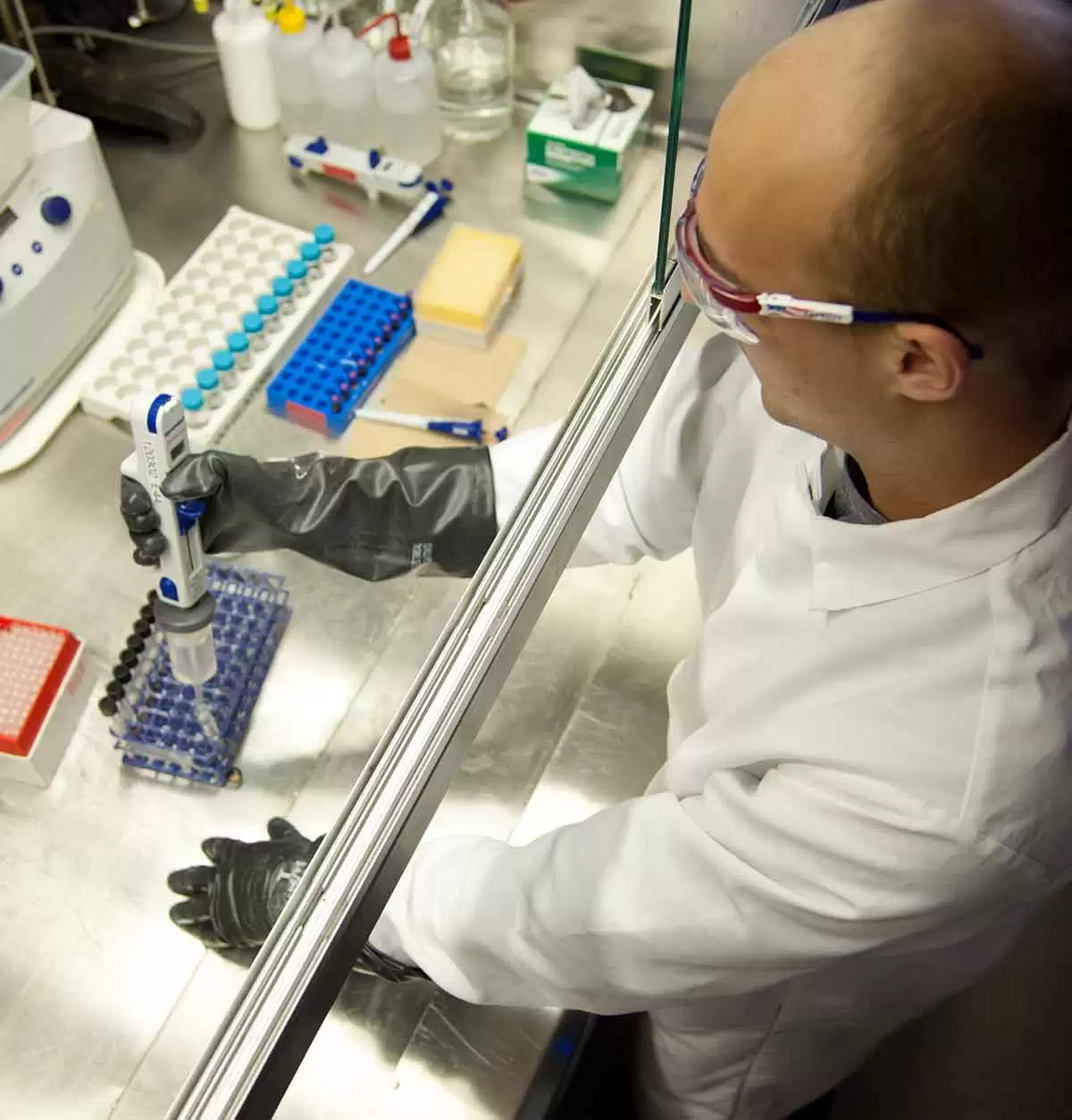
Creation of Celiac Disease Organoids
Researchers at Stanford Medicine developed a novel approach using organoids to model celiac disease. Organoids are three-dimensional cell cultures that mimic the structure and function of real organs. In this study, organoids were created from the intestinal tissue of individuals with celiac disease. These organoids include multiple cell types, such as epithelial cells, immune cells, and cells from the lining of the gut. This diversity allows the organoids to faithfully reproduce the interactions between different cell types seen in celiac disease patients.
The Role of IL-7 in Celiac Disease
Celiac.com Sponsor (A12):
The study revealed that interleukin-7 (IL-7), a molecule previously implicated in autoimmune diseases like rheumatoid arthritis and multiple sclerosis, plays a significant role in celiac disease. When gluten was introduced to the organoids derived from celiac patients, the researchers observed an increase in IL-7 levels, which was associated with immune activation and epithelial cell destruction. Blocking IL-7 activity prevented this damage, suggesting that IL-7 is a critical mediator of the immune response to gluten in celiac disease.
Findings and Implications
The researchers found that organoids from celiac patients, when exposed to gluten, showed an increase in IL-15 and the proliferation of CD4 T cells, which recognize gluten, and B cells, which produce antibodies to type 2 transglutaminase (TG2). This cascade of immune responses led to the activation of CD8 T cells that attack and kill epithelial cells. Blocking IL-7 activity in these organoids halted the epithelial destruction, indicating that IL-7 is a crucial factor in the disease mechanism. Furthermore, the study showed that IL-7 levels were elevated in biopsy samples from individuals with active celiac disease but not in those in remission on a gluten-free diet.
Significance for Celiac Disease Patients
The use of organoids provides a powerful new tool for understanding celiac disease at a cellular level. These models allow researchers to study the disease in ways that were not possible before, offering insights into the interactions between different cell types and the molecular mechanisms driving the immune response to gluten. The identification of IL-7 as a key player in celiac disease opens new avenues for potential therapeutic interventions. By targeting IL-7, it may be possible to develop treatments that mitigate the immune response to gluten and prevent the intestinal damage characteristic of celiac disease.
In conclusion, this study represents a significant advancement in the understanding of celiac disease. The ability to model the disease using organoids provides a platform for developing new drugs and personalized treatments. The discovery of IL-7's role in the disease process could lead to innovative therapies that improve the quality of life for individuals with celiac disease. The findings underscore the importance of continued research and the potential for organoid models to transform our approach to studying and treating autoimmune disorders.
Read more at: nature.com








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now