
Celiac.com 09/03/2018 - Can an office-based point of care test (POCT) improve celiac disease detection and diagnosis? A team of researchers recently set out to measure the diagnostic performance of an IgA/IgG-deamidated gliadin peptide (DGP)-based POCT for celiac disease detection, patient acceptability, and inter-observer variability of the POCT results.
The research team included Michelle S. Lau MBChB, Peter D. Mooney MD, William L. White MBChB, Michael A. Rees BMedSci, Simon H. Wong MBChB, Marios Hadjivassiliou FRCP, Peter H. R. Green MD, Benjamin Lebwohl MD & David S. Sanders FRCP. They are variously affiliated with the Academic Department of Gastroenterology, the Academic Department of Neurosciences and University of Sheffield, Royal Hallamshire Hospital, Sheffield Teaching Hospitals, Sheffield, UK, and with the Celiac Disease Centre at Columbia University Medical Centre in New York, NY, USA.
Celiac.com Sponsor (A12):
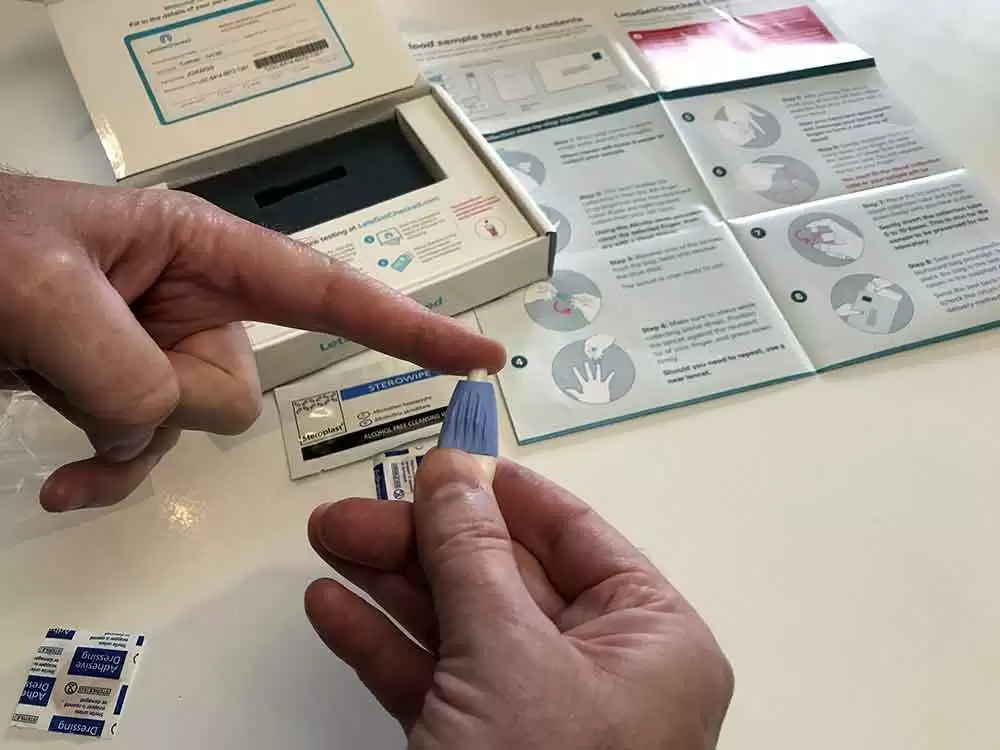
Beginning in 2013, and running through 2017, the team recruited patients who had been referred for secondary care with gastrointestinal symptoms, anemia and/or weight loss (group 1), along with a group of patients with self-reported gluten sensitivity, but unknown celiac disease status (group 2). Every patient in the study received a POCT, tests for IgA-tissue transglutaminase (IgA-TTG), IgA-endomysial antibodies (IgA-EMA), total IgA levels, and a duodenal biopsy.
A total of 500 patients completed acceptability questionnaires, and the team compared inter-observer variability of the POCT results among five clinical staff for 400 cases.
Group 1 included 1,000 patients. The team saw forty-one patients (4.1%) diagnosed with celiac disease. The sensitivities of the POCT, IgA-TTG, and IgA-EMA were 82.9, 78.1, and 70.7%; the specificities were 85.4, 96.3, and 99.8%. Group 2 included 61 patients. The POCT showed 100% sensitivity, but negative predictive value in detecting celiac disease in group 2.
A majority of patients preferred the POCT to a blood draw (90.4% to 2.8%). A Fleiss Kappa coefficient of 0.895 reflected good inter-observer agreement on the POCT results. The POCT had comparable sensitivity to a blood test, and accurately spotted all celiac disease cases in a gluten sensitive group. But, because its low specificity may could cause further unnecessary tests, it’s not good enough to take the place of blood testing.
It turns out that spotting celiac disease is only part of the battle. Making sure to rule out people who don’t have celiac disease is equally important. That’s why it’s important that any diagnostic test be both sensitive, to spot celiac disease, and specific, to rule out celiac disease in those who don’t have it.
Until we get a PCOT with high enough sensitivity and specificity to make accurate celiac diagnosis and accurate elimination of those without celiac disease, the current blood testing regime will continue.
Read more at: The American Journal of Gastroenterology; volume 113, pages1238–1246 (2018)






Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now