-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Our Content
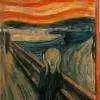
Short-Term Memory Problems
-
Get Celiac.com Updates:Support Celiac.com:
-
Celiac.com Sponsor (A17):
Celiac.com Sponsor (A17):
Celiac.com Sponsors (A17-M):
-
Recent Activity
-
- Oldturdle commented on Scott Adams's article in Spring 2025 Issue1
-
- Scott Adams replied to Jy11's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms15
Conflicting results
It's possible he's in the early stages of celiac disease, and it has been caught before villi damage. The blood test results so far do indicate possible celiac disease, as well as his strong family history of celiac disease. If his symptoms get better on a gluten-free diet this would be another strong indication. Personally I think it's definitely better... -
- Dora77 posted a topic in Post Diagnosis, Recovery & Treatment of Celiac Disease0
Permanent Floating & Undigested Stools for a Year
For some context: I have type 1 diabetes (T1D) (since 11 years) and celiac disease(since 4 years) For about a year now, I’ve been experiencing permanent floating and undigested stools. I’ve had a pancreas elastase test done. The first result was extremely low at 44, but a second test came back at 236. My doctor said that since one result is normal, it... -
- TerryinCO posted a topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms0
Status Update...
The Docs' and NP haven't committed to Celiac determination yet but say go gluten-free diet because... And I have with improved physical results - feeling better; overall functions better, and more energy. Still 10 pounds down in weight but I still have BMI of ~23. It's been just over a month now gluten-free diet. I'm fortunate I get along with diary/milk... -
- cristiana replied to Tyoung's topic in Post Diagnosis, Recovery & Treatment of Celiac Disease7
Increasing symptoms after going gluten free
I did suffer with gastric symptoms before diagnosis, but got all sorts of weird and wacky symptoms after going gluten free. Things got much better once my antibodies fell to normal levels, but it took years (please don't panic, many people's go to normal levels relatively quickly when following a gluten-free diet). Causes of the symptoms you mention...
-



Recommended Posts
Archived
This topic is now archived and is closed to further replies.