
Russ H
-
Posts
419 -
Joined
-
Last visited
-
Days Won
7
Content Type
Profiles
Forums
Events
Blogs
Celiac.com - Celiac Disease & Gluten-Free Diet Support Since 1995
Posts posted by Russ H
-
-
The problem with a a multiple screening test like this is that it is likely to generate at least one result that is outside the normal range in a healthy person leading to futile investigations. The pathogenesis of dermatitis herpetiformis makes it unlikely that someone would have raised IgA-tTG3 but not raised IgA-tTG2. Suspected dermatitis herpetiformis should be referred to a specialist for diagnosis. dermatitis herpetiformis causes a specific rash and symptoms - not merely hives.
-
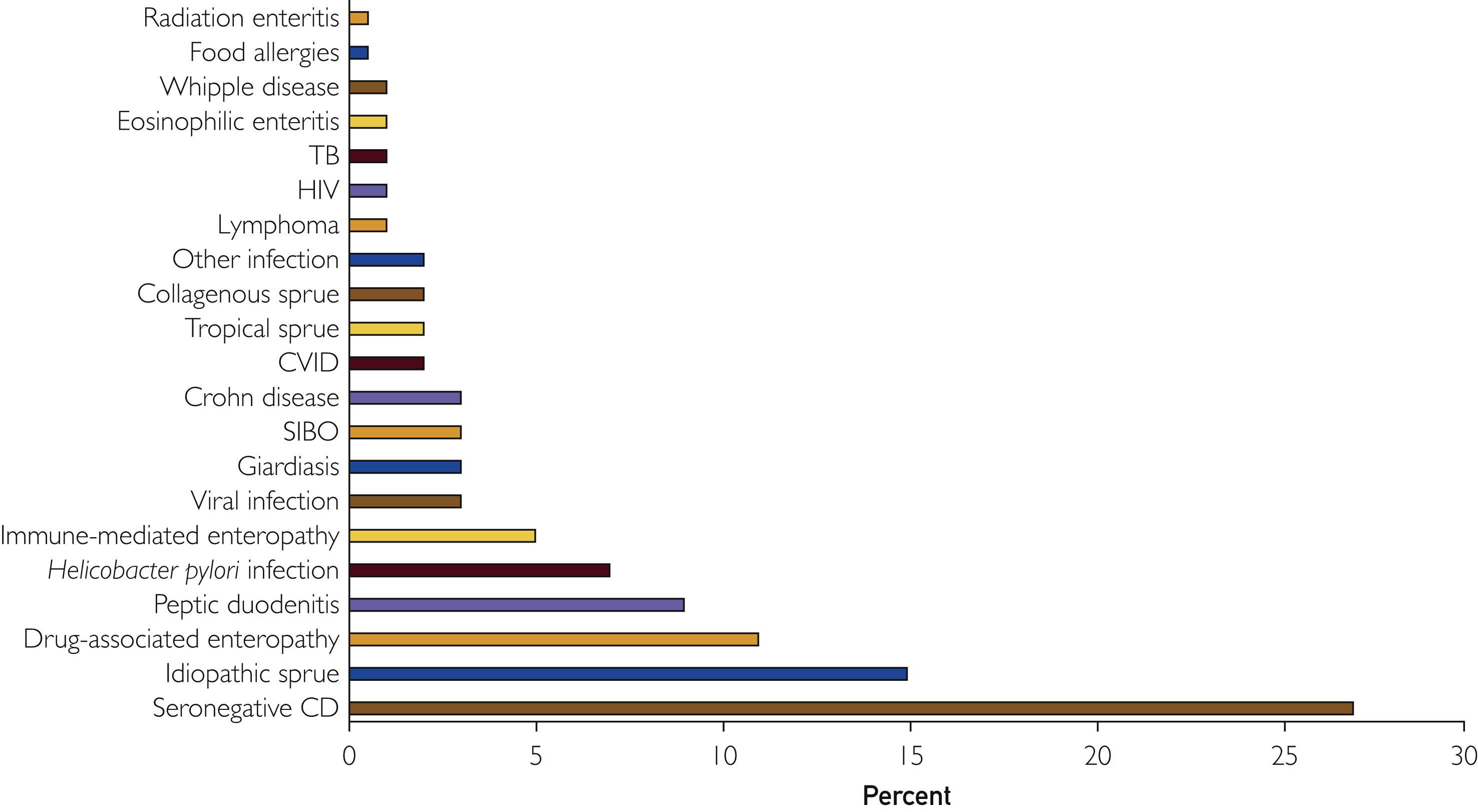
There is a good paper here on causes of seronegative villous blunting. The most common is seronegative coeliac disease.
Not All That Flattens Villi Is Celiac Disease: A Review of Enteropathies
- Scott Adams and knitty kitty
-
 1
1
-
 1
1
-
Sorry but I have to dash for an appointment so little time just now. Your signs and symptoms and response to a gluten-free diet sound like seronegative coeliac disease.
- knitty kitty and AllyJR
-
 1
1
-
 1
1
-
ohmichael, do you know that you've reacted to gluten? We all get ups and downs in health - a mild viral infection one week and maybe an unset stomach another time. It is easy to ascribe the symptoms to gluten exposure even when that is not the cause of the symptoms. I would wait and see if it happens again before giving up your job, especially if you don't have another one to go to.
-
People with coeliac disease tend to have lower systolic blood pressure. However symptoms vary greatly between people and there are multiple cases in the literature of hypertension in people diagnosed with coeliac disease that gradually reverses on a strict gluten-free diet.
-
There is not enough information to assess the likelihood of coeliac disease. You'll have to chase this up with the quack. The lab should provide antibody titres and a reference range. They might just have done an EMA test, which is negative/positive and antiquated - a proper IgA-ttG2 test would be more helpful.
-
I developed a heart arrhythmia and on several occasions had to wear a 24 hour Holter monitor. Among other things, I had premature atrial complexes (PACs) and occasional AFib. I was very fit at the time, running and cycling. This completely disappeared following my diagnosis and following a strict gluten free diet. I haven't had a single episode since, in 4 years.
- cristiana and Scott Adams
-
 2
2
-
3 hours ago, trents said:
Some cultivars of oats actually contain gluten.
I have read research indicating differing reactions to various oat cultivars, however, nothing suggesting that some contain gluten - do you have a source for that?
-
Hi Cosyfeyre and welcome to the forum.
Hashimoto's thyroiditis can cause moderately raised levels of tissue transglutaminase antibodies (as can other autoimmune and inflammatory conditions). This could explain the weak positive shown for tTG IgG. It is certainly worth following up. Some people can react to gluten without having coeliac disease, and many people react to the fructans present in grains like wheat.
-
It can take between 6 months and 2 years for the dermatitis herpetiformis rash to resolve. The symptoms of dermatitis herpetiformis arise from deposits of certain antibodies building up in the skin. These deposits attract immune cells leading to inflammation and blistering. It can take 10 years for the deposits to be reabsorbed although symptoms resolve long before this.
-
Your initial test showed a moderately raised level of IgA tTG2. There are several causes of this apart from coeliac disease including: inflammation of the joints, bowel and liver. Transient rise in levels can be caused by an infection.
-
Small amounts of gliadin are detectable in some samples of human breast milk but these are at too low a level to cause symptoms. No gliadin has been detected in the beef of grain-fed cattle.
-
I doubt very much that it contains any gluten. It works by producing an artificial blood clot, mixing 2 or more proteins found in the natural blood clotting cascade. These are refined from human blood donations. It comes in 2 vials that are mixed immediately before use and clot quickly.
-
Apart from the symptoms of SIBO there may be other symptoms that you are unaware of because they come on so slowly. It takes a long time to fully recover, especially when diagnosed as an adult. Apart from the classic signs and symptoms, I had all sorts of strange ones that have gradually resolved including: heart arrhythmia, tendonitis, chilblains, body odour, painful scalp, memory problems and thickened red skin on knees and elbows. It is definitely worth getting a diagnosis and following a strict gluten free diet.
-
The prevalence of SIBO is about 5x higher in people with coeliac disease than those without. In people with coeliac disease, it responds well to antibiotic therapy. It can take several years to achieve full recovery of the digestive tract when following a strict gluten free diet.
Note that if you are having a biopsy to confirm coeliac disease, you must continue eating gluten prior to the test. Clinical guidance in the UK is to eat at least 2 gluten-containing meals every day for at at 6 weeks prior to testing. US guidance will be similar. In the UK, if your blood antibody levels are at least 10x standard range and you are under 55, you can be diagnosed on blood test results alone.
-
Note also that the amount of problematic protein (gliadin) that is found in breast milk of women having a normal gluten containing diet varies but is very small. Although the study referenced below says 'very high', the amounts detected vary between undetectable and a maximum of 1.2 parts per million. Breast milk is considered safe for infants with coeliac disease even if the mother consumes gluten.
-
Hello, and welcome to the forum. More knowledgable people might be able to chime in. Firstly, coeliac disease causes all sorts of bizarre manifestations in adults from chilblains to schizophrenia. There is a direct association between coeliac disease and arthritis in younger people, and coeliac disease has a common genetic predisposition with rheumatoid arthritis. It is certainly possible that your joint problems are related to coeliac disease, particularly if they manifest after consuming gluten. I rarely eat out anymore because I don't trust the kitchens, so I understand the effect of social events. It is hard at first but stick with it and you will get used to it and feel much better for it - it can take several years to fully recover in adults.
8 hours ago, Jean Shifrin said: -
An interesting presentation from 2023 concerning the effects of consuming purified avenin protein from oats. From my understanding of this study, people with coeliac disease do have T-cells that recognise and react to oats. However:
1. 38% of participants with coeliac initially developed raised blood inflammatory markers following consumption of avenin.
2. 62% developed at least one symptom (vomiting, headache, lethargy etc.).
3. Worse symptoms correlated with greater level of blood inflammatory marker (IL2).
4. Over 6 weeks there was no histologic damage or evidence of serologic disease and the immune response to avenin markedly fell.
5. Tolerance of oat avenin developed over 1-2 weeks, and symptoms disappeared.
6. 1 person of the 29 who participated in the study developed a wheat-type immunological response to avenin and had to leave the study.
The study supports the opinion that a subset of people with coeliac disease cannot tolerate oats at all and develop a coeliac-type response to avenin. It also suggests that most people with coeliac disease can tolerate oats without provoking villus blunting or raised serologic markers.
Oats in Coeliac Disease, Coeliac UK Research Conference 2023
-
You should be careful with anything containing oats (such as granola) unless they are specifically gluten-free. Oats are often contaminated due to various factors including crop rotation, adjacent crops and the sharing of harvesting and milling equipment. Barley malt extracts can be up to 1000 ppm of gluten unless certified gluten free. Even though only a small amount would be used for flavouring, I think this should be avoided.
Thanks for the M&S suggestion.
-
Approximately 1 in 3 adults have neurological symptoms on diagnosis. The mechanism and pathogenesis is unknown. These normally go into remission on a strict gluten-free diet. Common symptoms are anxiety, slow thinking, 'brain fog', memory problems and headaches. Although I think I have had coeliac disease in a mild form since childhood, my symptoms suddenly became much worse in later life. Along with the gastrointestinal symptoms and fatigue, I developed a tremendous sense of doom, anxiety and paranoia.
The diet can be awkward at first but becomes easier with time.
-
For those in the UK wondering whether a diagnosis of coeliac disease alone makes one eligible for a 2024 Autumn COVID booster, it seems that yes, this does make one eligible. There is variability between GP surgeries in proactively calling people in for vaccination, but it is straightforward to use the NHS App to book a vaccination. If attending a pharmacy you might have to point out the information to the pharmacist. I have had no problem receiving vaccinations at nurse-led drop-in centres or GP surgeries but did have an awkward pharmacist on one occasion.
According to the UK Health Security Agency, COVID vaccination is offered to (ignoring other qualifying criteria):
Quoteindividuals aged 6 months to 64 years in a clinical risk group (as defined in tables 3 or 4 in the COVID-19 chapter of the Green Book)
UKHSA, Who’s eligible for the 2024 COVID-19 vaccine, or ‘Autumn Booster’?
According to Table 3 of Chapter 14a of the Green Book, coeliac disease is a risk group:
QuoteAsplenia or dysfunction of the spleen: This also includes conditions that may lead to splenic dysfunction, such as homozygous sickle cell disease, thalassemia major and coeliac syndrome
COVID-19: the green book, chapter 14a
Approximately 30% of people with coeliac disease are hyposplenic - it is more common in those diagnosed in adulthood than childhood.
-
7 hours ago, JForman said:
At this point, now Sept 2024, she is having stool accidents daily (sometimes multiple times per day). The stool, when it does leak out, is not typical "constipation rocks" - it's colored normally, no mucous, but STICKY and thick. Most of the time we have to use wet wipes or get in the shower to clean her off. She has bouts of acid reflux, but not often. No complaints of stomach pain.
This could be steatorrhoea (fatty stools), which is a common symptom of coeliac disease due to fat malabsorption. Easy to perform a lab test for. Reflux is also a common symptom of untreated coeliac disease.
I think trents is correct that a total-IgA test is needed to rule out IgA deficiency.
-
Those serum tests are for total immunoglobulins in each class (IgA and IgM) and are not specific to coeliac disease. You need the test results for antibodies to tTG2, which is a very sensitive test for coeliac disease. I would follow your doctor's advice.
-
Interesting study on gluten cross-contamination. Biggest risk from pasta water, pots and utensils. Toasters surprisingly not!

Confused about my results
in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Posted
There is a predictive model for children on this link. Depends on sex, HLA genes and number of affected close relatives. The model only goes up to age 12 so it would be interesting to know what the lifetime risk is.
https://hputter.shinyapps.io/preventcd/