
Russ H
-
Posts
400 -
Joined
-
Last visited
-
Days Won
6
Content Type
Profiles
Forums
Events
Blogs
Celiac.com - Celiac Disease & Gluten-Free Diet Support Since 1995
Posts posted by Russ H
-
-
Hello, and welcome to the forum. More knowledgable people might be able to chime in. Firstly, coeliac disease causes all sorts of bizarre manifestations in adults from chilblains to schizophrenia. There is a direct association between coeliac disease and arthritis in younger people, and coeliac disease has a common genetic predisposition with rheumatoid arthritis. It is certainly possible that your joint problems are related to coeliac disease, particularly if they manifest after consuming gluten. I rarely eat out anymore because I don't trust the kitchens, so I understand the effect of social events. It is hard at first but stick with it and you will get used to it and feel much better for it - it can take several years to fully recover in adults.
8 hours ago, Jean Shifrin said: -
An interesting presentation from 2023 concerning the effects of consuming purified avenin protein from oats. From my understanding of this study, people with coeliac disease do have T-cells that recognise and react to oats. However:
1. 38% of participants with coeliac initially developed raised blood inflammatory markers following consumption of avenin.
2. 62% developed at least one symptom (vomiting, headache, lethargy etc.).
3. Worse symptoms correlated with greater level of blood inflammatory marker (IL2).
4. Over 6 weeks there was no histologic damage or evidence of serologic disease and the immune response to avenin markedly fell.
5. Tolerance of oat avenin developed over 1-2 weeks, and symptoms disappeared.
6. 1 person of the 29 who participated in the study developed a wheat-type immunological response to avenin and had to leave the study.
The study supports the opinion that a subset of people with coeliac disease cannot tolerate oats at all and develop a coeliac-type response to avenin. It also suggests that most people with coeliac disease can tolerate oats without provoking villus blunting or raised serologic markers.
Oats in Coeliac Disease, Coeliac UK Research Conference 2023
-
You should be careful with anything containing oats (such as granola) unless they are specifically gluten-free. Oats are often contaminated due to various factors including crop rotation, adjacent crops and the sharing of harvesting and milling equipment. Barley malt extracts can be up to 1000 ppm of gluten unless certified gluten free. Even though only a small amount would be used for flavouring, I think this should be avoided.
Thanks for the M&S suggestion.
-
Approximately 1 in 3 adults have neurological symptoms on diagnosis. The mechanism and pathogenesis is unknown. These normally go into remission on a strict gluten-free diet. Common symptoms are anxiety, slow thinking, 'brain fog', memory problems and headaches. Although I think I have had coeliac disease in a mild form since childhood, my symptoms suddenly became much worse in later life. Along with the gastrointestinal symptoms and fatigue, I developed a tremendous sense of doom, anxiety and paranoia.
The diet can be awkward at first but becomes easier with time.
-
For those in the UK wondering whether a diagnosis of coeliac disease alone makes one eligible for a 2024 Autumn COVID booster, it seems that yes, this does make one eligible. There is variability between GP surgeries in proactively calling people in for vaccination, but it is straightforward to use the NHS App to book a vaccination. If attending a pharmacy you might have to point out the information to the pharmacist. I have had no problem receiving vaccinations at nurse-led drop-in centres or GP surgeries but did have an awkward pharmacist on one occasion.
According to the UK Health Security Agency, COVID vaccination is offered to (ignoring other qualifying criteria):
Quoteindividuals aged 6 months to 64 years in a clinical risk group (as defined in tables 3 or 4 in the COVID-19 chapter of the Green Book)
UKHSA, Who’s eligible for the 2024 COVID-19 vaccine, or ‘Autumn Booster’?
According to Table 3 of Chapter 14a of the Green Book, coeliac disease is a risk group:
QuoteAsplenia or dysfunction of the spleen: This also includes conditions that may lead to splenic dysfunction, such as homozygous sickle cell disease, thalassemia major and coeliac syndrome
COVID-19: the green book, chapter 14a
Approximately 30% of people with coeliac disease are hyposplenic - it is more common in those diagnosed in adulthood than childhood.
-
7 hours ago, JForman said:
At this point, now Sept 2024, she is having stool accidents daily (sometimes multiple times per day). The stool, when it does leak out, is not typical "constipation rocks" - it's colored normally, no mucous, but STICKY and thick. Most of the time we have to use wet wipes or get in the shower to clean her off. She has bouts of acid reflux, but not often. No complaints of stomach pain.
This could be steatorrhoea (fatty stools), which is a common symptom of coeliac disease due to fat malabsorption. Easy to perform a lab test for. Reflux is also a common symptom of untreated coeliac disease.
I think trents is correct that a total-IgA test is needed to rule out IgA deficiency.
-
Those serum tests are for total immunoglobulins in each class (IgA and IgM) and are not specific to coeliac disease. You need the test results for antibodies to tTG2, which is a very sensitive test for coeliac disease. I would follow your doctor's advice.
-
Interesting study on gluten cross-contamination. Biggest risk from pasta water, pots and utensils. Toasters surprisingly not!
-
3 minutes ago, olioil said:
Thank you Russ and also everyone else in the thread! I'll definitely cut out oats, and I'll be patient when waiting for symptoms to subside. I read about celiacs feeling better "immediately" which scared me that I was doing something wrong, but it makes me feel a lot better that it takes a while for everything to calm down. I'll take oats out and be cautious about cross contact while trying to heal. Seriously appreciate the advice from everyone.
I have a diary somewhere but if I recall correctly, I began to notice an improvement after about 2 weeks, but that is a slight improvement. The major one was 3 months in.
I think I had it for at least 45 years prior to diagnosis. I am 3 years in and I think I am still recovering. Most of the recovery was in the first year, by which time I was back on the rails and functional, if a little traumatised by the experience. The dietary restrictions are quite tough practically and socially. Breadth and severity of symptoms vary hugely between individuals.
It is definitely worth taking a good multivitamin for the first year at least as most people on diagnosis have at least one vitamin/mineral deficiency.
-
On 8/25/2024 at 4:29 PM, carolcat said:
I was wondering about that but then guess since it mostly is asymptomatic then it never acted up enough to make me think about getting checked, and all those years flew by.
Thank u for bringing that up.
You might notice that you were actually symptomatic but you were just habituated to the symptoms. I had all kinds of strange signs and symptoms that just disappeared such as red thickened skin on knees and elbows, chilblains, body odour, tendonitis and a heart arrhythmia amongst others.
-
1 hour ago, olioil said:
Hi Scott,
Thanks for your kind reply. I have a follow-up appointment with my GI pretty soon so I'll try and speak with them regarding those deficiencies. Maybe I can get tested or I can look into good supplements that are totally gluten-free.And to the best of my knowledge, I am 100% gluten-free. I tried to do as much research as possible to make sure I'm not getting any cross contact, but I am in a shared kitchen so I can only control my own actions. I have only been 100% gluten-free for around a week or two though (For like another week beforehand I was gluten-free but still using shared kitchen equipment). I guess it's too early to tell anything, it's just disheartening to feel worse after trying to put effort into being gluten free.
The generally accepted as safe level of gluten for people with coeliac disease is 10 mg (although some people are more sensitive and some people less). This is equivalent to a piece of bread the size of a small pea. Even with shared utensils, you can prepare safely so long as you make sure everything is clean. Stainless steel and non-stick pans are easy to keep clean. Don't share unglazed cast iron cookware as the rough surface traps food. Don't share the toaster - use toasting pouches if you have to. Also, watch out for forks and make sure to clean between the tines.
People with active coeliac disease often react to other foods because the gut barrier is damaged and also because the antibodies to gluten they make as part of the disease can cross-react to other foods. This reaction generally fades as the gut heals and antibody levels falls but this can take a year or more. Note that you can still have coeliac antibodies but they remain in the gut wall without escaping into the bloodstream, so causing a negative blood test.
It took 3 months for my bloating, burping and reflux to resolve, other symptoms even longer.
Edit: Definitely cut out oats. When the disease has fully gone into remission, try reintroducing them to see if you react. In most people (90-95%) oats don't trigger the coeliac disease immune response. However, the antibodies generated by consuming gluten do cross react with oat protein (avenin). You need to wait until the disease has gone into remission to find out whether you react to oats.
-
This is totally false. Gluten is the name for the protein found in wheat, barley and rye flour. When wheat flour is worked into dough, it is the gluten that makes it stretchy and elastic. Adding oil may alter the properties of the flour when it is worked, but it won't affect the actual gluten content.
-
It may be worth getting yourself tested for coeliac disease as a 1st degree relative of someone with the condition has an increased chance of having coeliac disease (about 10%).
-
6 hours ago, trents said:
Is he consuming dairy? About 10% of celiacs react to the protein casein in dairy like they do the protein gluten in wheat/barley/rye. The structures are very similar.
My understanding is that this is a cross-reaction - people with active coeliac disease generate antibodies that cross-react to milk proteins amongst other things. However, the cross-reaction does not drive coeliac disease, and when gluten is excluded and the antibodies fade out, the cross reaction disappears.
-
An optimistic article from the journal Nature about emerging therapies for autoimmune diseases.
Nature: Can autoimmune diseases be cured? Scientists see hope at last
QuoteAfter decades of frustration and failed attempts, scientists might finally be on the cusp of developing therapies to restore immune ‘tolerance’ in conditions such as diabetes, lupus and multiple sclerosis.
-
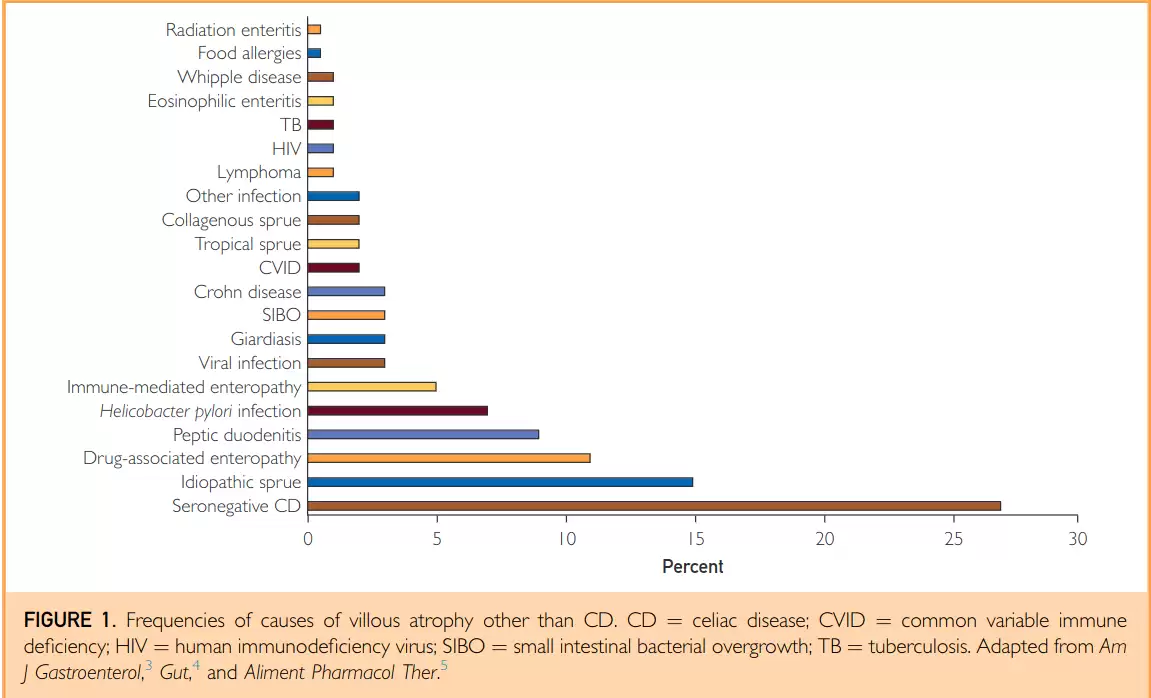
I thought this clinical review might be of interest. Coeliac disease followed by seronegative coeliac disease are the most common causes of villi flattening. Other causes include idiopathic sprue, drug-associated enteropathy, peptic duodenitis and helicobacter among 20 or so known conditions.
Not All That Flattens Villi Is Celiac Disease: A Review of Enteropathies
-
23 hours ago, lmemsm said:
20 minutes isn't bad for a bread recipe. It's been taking me much longer for the gluten-free ones I've tried so far. That was one reason I wanted to see if I could use the bread machine for this, to speed things up. I read substituting powder for psyllium husk isn't one to one. I've seen a figure of 85% in a few places. Thought this was a helpful article: https://theloopywhisk.com/2021/10/23/psyllium-husk-101/
Thanks for the link. I follow a low sodium diet, so baking my own bread is unavoidable. I use lo-salt, which is 2/3 potassium chloride and 1/3 sodium chloride. Doesn't affect the dough rise and gives normal flavour to the bread.
-
8 minutes ago, lmemsm said:
Thanks for the tips on psyllium husk. I'll have to look for the whole husk. I'm using the powder from nuts.com. Haven't noticed a color change from it. It'll be interesting to try the whole powder and see how the results compare.
I think it might be to do with whether the pure husk or more of the seed is used to make the powder. I tried powdering the husks in a small coffee grinder but they absorbed too much water and the mix became dry, then I added water and it didn't bake as well. The recipe I linked to above is quite time consuming to prepare but makes really nice bread. I have played around with it a bit - I don't use flax but I add 75g (3 oz) of mixed seeds. I beat 3 large eggs and add milk to make 510g. I use digital scales for all ingredients. Takes me 20 minutes to mix up and clean up. Luckily I don't seem to react to pure oats.
-
In the UK, NICE guidelines state that people with type 1 diabetes should be offered testing for coeliac disease on diagnosis as they share a common genetic predisposition.
-
On 1/22/2024 at 4:18 PM, lmemsm said:
I ended up buying the Panasonic. Am having trouble finding bread recipes that I'd like to try in it. I did find one that I thought came out better than the commercial gluten-free bread I've tried: https://www.cookingwithcamilla.com/vegan-gluten-free-bread-machine-loaf/ Still looking for others that use ingredients I don't have issues with. It's not as easy to make gluten free bread in a bread machine as it is to make regular bread, but it does seem easier than making the bread completely from scratch.
Try the Gluten Free Alchemist website I linked to above. She has quite a few recipes. I found the key thing to replace gluten is psyllium seed husk. You have to get the right type of psyllium - don't get powder, get whole husk. I have found the powder turns purple when baked, it also absorbs lots of water and is difficult to get the recipe right. You need whole 'golden' husk. The one I use is below:
-
That is very interesting. It look like anti-tTG3 antibodies originating in the gut bind to tTG3 in the skin, forming complexes. Iodine leads to structure alterations promoting aberrant behaviour of tTG3 and promotion of disease activity.
-
1 hour ago, Raquel2021 said:
I completely undertand. It took me months to realize it was the eggs and dairy causing my paresthesia but eliminated them out of desperation. Lastly my endocrinologist told me Hashimotos patients do better with no iodized salt but I didn't listen as I know iodine is needed but as I said that was what made the difference. Basically I am on a low iodine diet as iodine is in everything. Just eggs, dairy and iodized salt are big on iodine.
Do your own research. Iodine affects patients with DH.
Eggs and oats won't raise tTG2 antibodies. Are the oats certified gluten free?
-
On 1/5/2024 at 5:44 AM, Berkan said:
Hey! I just checked my results now before I go to my doctor appointment again and I just saw my
Anti-Gliadin Ab.IgG is 35. but all the others are low. I had all the symptoms of celiac, that's why
doctor wanted that. All I want to ask to you guys, is 35 something to concern?
It is certainly worth following up if your have persistent symptoms. Was your total IgA measured as part of the coeliac screening test?
-
On 1/5/2024 at 5:44 AM, Berkan said:
Hey! I just checked my results now before I go to my doctor appointment again and I just saw my
Anti-Gliadin Ab.IgG is 35. but all the others are low. I had all the symptoms of celiac, that's why
doctor wanted that. All I want to ask to you guys, is 35 something to concern?
You have isolated positive anti-DGP: in the absence of a person having IgA deficiency, this has poor positive predictive value for coeliac disease - 15.5% (95% CI 8.5–25.0%). This is because it is not unusual for people without coeliac disease to have DGP antibodies.

Pretty desperate for some guidance
in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Posted
Note also that the amount of problematic protein (gliadin) that is found in breast milk of women having a normal gluten containing diet varies but is very small. Although the study referenced below says 'very high', the amounts detected vary between undetectable and a maximum of 1.2 parts per million. Breast milk is considered safe for infants with coeliac disease even if the mother consumes gluten.
https://pubmed.ncbi.nlm.nih.gov/9867098/