Russ H
Moderators-
Posts
446 -
Joined
-
Last visited
-
Days Won
8
Content Type
Profiles
Forums
Events
Blogs
Latest Celiac Disease News & Research:
Everything posted by Russ H
-
Interesting study on gluten cross-contamination. Biggest risk from pasta water, pots and utensils. Toasters surprisingly not! Preparation of Gluten-Free Foods Alongside Gluten-Containing Food May Not Always Be as Risky for Celiac Patients as Diet Guides Suggest
-
I have a diary somewhere but if I recall correctly, I began to notice an improvement after about 2 weeks, but that is a slight improvement. The major one was 3 months in. I think I had it for at least 45 years prior to diagnosis. I am 3 years in and I think I am still recovering. Most of the recovery was in the first year, by which time I was back on...
-
Diagnosed at 79 - 3/4 years old
Russ H replied to carolcat's topic in Post Diagnosis, Recovery & Treatment of Celiac Disease
You might notice that you were actually symptomatic but you were just habituated to the symptoms. I had all kinds of strange signs and symptoms that just disappeared such as red thickened skin on knees and elbows, chilblains, body odour, tendonitis and a heart arrhythmia amongst others. -
Gluten as a Proinflammatory Inducer of Autoimmunity in Everyone
Russ H commented on Scott Adams's article in Autumn 2024 Issue
It would be interesting to look at populations that have never been exposed to gluten.- 7 comments
-
- autoimmune diseases
- celiac disease
- (and 6 more)
-
The generally accepted as safe level of gluten for people with coeliac disease is 10 mg (although some people are more sensitive and some people less). This is equivalent to a piece of bread the size of a small pea. Even with shared utensils, you can prepare safely so long as you make sure everything is clean. Stainless steel and non-stick pans are easy to...
-
What Causes Villous Atrophy Besides Celiac Disease?
Russ H commented on Scott Adams's article in Additional Concerns
Lactose-free milk is readily available in the UK. https://www.tesco.com/groceries/en-GB/shop/fresh-food/milk-butter-and-eggs/milk/lactose-free-milk- 13 comments
-
This is totally false. Gluten is the name for the protein found in wheat, barley and rye flour. When wheat flour is worked into dough, it is the gluten that makes it stretchy and elastic. Adding oil may alter the properties of the flour when it is worked, but it won't affect the actual gluten content.
-
Is Depression Really a Chemical Imbalance?
Russ H commented on Dr. Vikki Petersen D.C, C.C.N's article in Spring 2009 Issue
I experienced memory problems, brain fog and anxiety. Gradually faded on a gluten free diet and came back with a vengeance when I resumed eating gluten for testing.- 3 comments
-
- anxiety
- celiac disease
- (and 4 more)
-
My understanding is that this is a cross-reaction - people with active coeliac disease generate antibodies that cross-react to milk proteins amongst other things. However, the cross-reaction does not drive coeliac disease, and when gluten is excluded and the antibodies fade out, the cross reaction disappears.
-
The paper is currently freely available: Characterizations of a neutralizing antibody broadly reactive to multiple gluten peptide:HLA-DQ2.5 complexes in the context of celiac disease
- 5 comments
-
- celiac disease
- chugai
-
(and 3 more)
Tagged with:
-
Rise in Fatal Celiac-Related Cancer Alarms Researchers
Russ H commented on Jefferson Adams's article in Cancer, Lymphoma and Celiac Disease
It would normally be diagnosed by a combination of endoscopy and biopsy findings combined with blood tests for coeliac disease related antibodies.- 13 comments
-
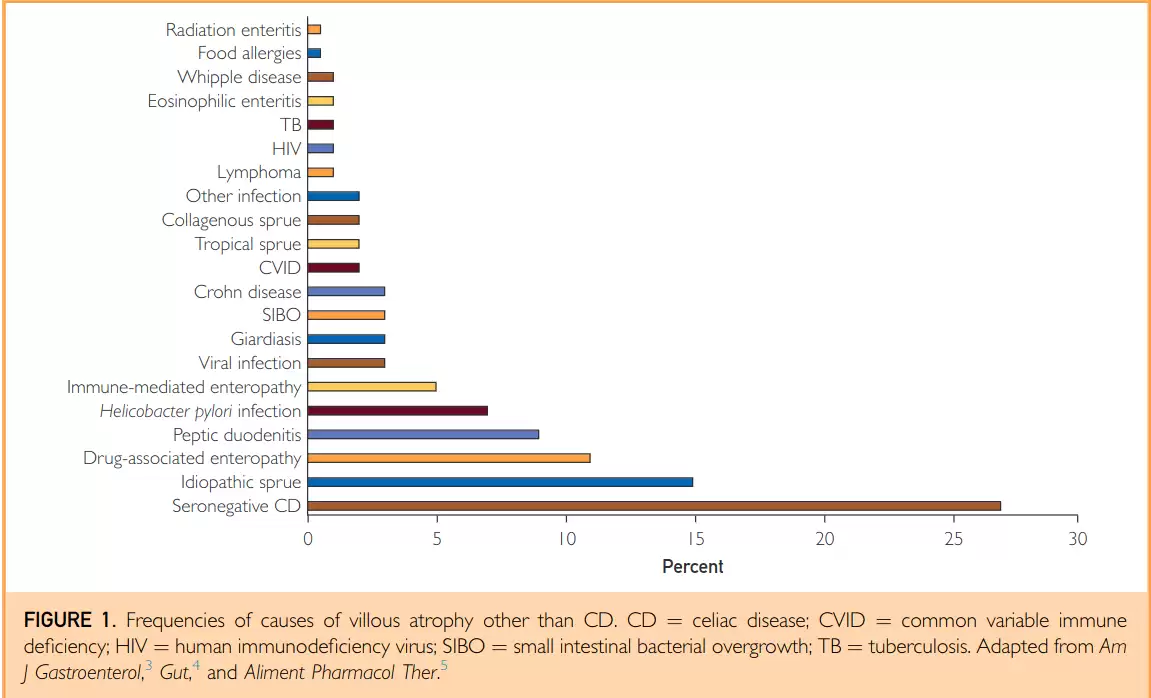
I thought this clinical review might be of interest. Coeliac disease followed by seronegative coeliac disease are the most common causes of villi flattening. Other causes include idiopathic sprue, drug-associated enteropathy, peptic duodenitis and helicobacter among 20 or so known conditions. Not All That Flattens Villi Is Celiac Disease: A Review of...
-
Is it worth buying a bread machine?
Russ H replied to lmemsm's topic in Gluten-Free Recipes & Cooking Tips
Thanks for the link. I follow a low sodium diet, so baking my own bread is unavoidable. I use lo-salt, which is 2/3 potassium chloride and 1/3 sodium chloride. Doesn't affect the dough rise and gives normal flavour to the bread. -
Is it worth buying a bread machine?
Russ H replied to lmemsm's topic in Gluten-Free Recipes & Cooking Tips
I think it might be to do with whether the pure husk or more of the seed is used to make the powder. I tried powdering the husks in a small coffee grinder but they absorbed too much water and the mix became dry, then I added water and it didn't bake as well. The recipe I linked to above is quite time consuming to prepare but makes really nice bread. I have... -
Celiac or just losing my mind?
Russ H replied to Toparsenalfan's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
In the UK, NICE guidelines state that people with type 1 diabetes should be offered testing for coeliac disease on diagnosis as they share a common genetic predisposition. -
Is it worth buying a bread machine?
Russ H replied to lmemsm's topic in Gluten-Free Recipes & Cooking Tips
Try the Gluten Free Alchemist website I linked to above. She has quite a few recipes. I found the key thing to replace gluten is psyllium seed husk. You have to get the right type of psyllium - don't get powder, get whole husk. I have found the powder turns purple when baked, it also absorbs lots of water and is difficult to get the recipe right. You need... -
Speaking as someone who has lived in Sweden for several years on different occasions, Sweden is an absolute nightmare for people with coeliac disease. The whole of Scandinavia is bad but Sweden is the worst. It is just Lutheran culture - you are burden on society, and they don't care. Italy is fantastic, they worship food. France, Germany good. Amazingly...
- 11 comments
-
That is very interesting. It look like anti-tTG3 antibodies originating in the gut bind to tTG3 in the skin, forming complexes. Iodine leads to structure alterations promoting aberrant behaviour of tTG3 and promotion of disease activity. https://pdf.sciencedirectassets.com/271007/1-s2.0-S0022202X18X00098/1-s2.0-S0022202X18317263/main.pdf
-
Blood Test Result
Russ H replied to Berkan's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
It is certainly worth following up if your have persistent symptoms. Was your total IgA measured as part of the coeliac screening test? -
Blood Test Result
Russ H replied to Berkan's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
You have isolated positive anti-DGP: in the absence of a person having IgA deficiency, this has poor positive predictive value for coeliac disease - 15.5% (95% CI 8.5–25.0%). This is because it is not unusual for people without coeliac disease to have DGP antibodies. https://celiacdiseasecenter.columbia.edu/wp-content/uploads/2018/12/Diagnostic-Yield-o...