Russ H
Moderators-
Posts
420 -
Joined
-
Last visited
-
Days Won
7
Content Type
Profiles
Forums
Events
Blogs
Celiac.com - Celiac Disease & Gluten-Free Diet Support Since 1995
Everything posted by Russ H
-
Creating a Celiac Safe Kitchen
Russ H replied to Stacy Nelson's topic in Gluten-Free Foods, Products, Shopping & Medications
Could you share your test results? Values and reference ranges. Most people with coeliac disease can tolerate 10 mg of gluten a day without provoking an immune response. This is the generally accepted as safe level. Wheat flour is about 10% protein, so 10 mg gluten is about 100 mg of wheat flour. Bread has a specific gravity of about 0.25, giving a volume... -
It refers to data presented at https://ddw.org/ . Possibly a poster presentation although I can't find it anywhere. The author is interviewed in the link below and suspects that problems could be related to non-adherence to a strict gluten-free diet. https://www.hcplive.com/view/jansson-knodell-treating-pregnant-women-celiac-disease
- 18 comments
-
- celiac disease
- complication
-
(and 6 more)
Tagged with:
-
Celiac Disease And High Blood Pressure...
Russ H replied to Sheryl in NJ's topic in Related Issues & Disorders
It is not unheard of. https://www.nature.com/articles/1001404 -
Avoid Gluten with Elevated Antibodies but No Celiac Disease?
Russ H commented on Dr. Tom O'Bryan's article in Winter 2008 Issue
Isolated positive DGP-IgG has very poor predictive value for coeliac disease in adults. It is useful in infants.- 3 comments
-
- antibodies
- avoid
- (and 6 more)
-
I was ill for so long that I don't remember what normal is. I think I was ill for more than 40 years. I was diagnosed over 2 years ago. I was totally intolerant to dairy but this has now gone. I probably have a lingering dysbiosis and some foods such as beans cause a lot of bloating and burping. Your iron seems very low. Do you take vitamin C with it...
-
I do the same thing. Mercifully, I don't go into anaphylaxis as some people do if exposed to allergens, but on the other hand don't know whether I have been exposed enough to provoke an immune response and all the sequelae that involves. Apart from a handful of local places that I know are safe, I don't eat out. I got badly glutened several times in Sweden...
- 17 comments
-
People here a posting rigorous scientific consensus backed information. Kennedy is not.
- 19 comments
-
- connection
- gluten
-
(and 3 more)
Tagged with:
-
I doubt that very much. Robert F Kennedy jr. has no scientific or medical qualifications and promotes conspiracy theories and anti-vaccine propaganda. Childhood vaccines do not cause problems for most people - they are thoroughly tested and monitored and are very safe. It is not known what triggers coeliac disease. The allegation that glyphosphate causes...
- 19 comments
-
- connection
- gluten
-
(and 3 more)
Tagged with:
-
Dairy Free Baby Formula
Russ H replied to jwhitty's topic in Parents, Friends and Loved Ones of Celiacs
Exactly. Undigested proteins are excreted in the stool, they don't get into the meat or dairy products. -
Researchers Seek the Holy Grail of Gluten-Free Bread
Russ H commented on Jefferson Adams's article in Summer 2023 Issue
I got myself a bread machine and found a good recipe based upon gluten-free oat flour amongst other ingredients. It uses psyllium husk to replace the gluten and the result is just like wheat bread. https://www.glutenfreealchemist.com/gluten-free-bread-machine-recipe-bread-maker/- 4 comments
-
Strange diagonal creases on forearm
Russ H replied to Simmons15's topic in Related Issues & Disorders
These forearm creases seem to be caused by WHB rather than coeliac disease and go into spontaneous remission after sufficient time. (WHB = women holding babies). -
The enzyme has been approved by the European Food Safety Agency as safe for regular human consumption: https://www.efsa.europa.eu/en/efsajournal/pub/4681 They tend to follow the precautionary principle, so if they regard it as safe it probably is.
-
Would be interesting to see whether vaccination against Strep. pneumoniae affects incidence of coeliac disease. In the UK, it has been given to infants since 2006 so I suppose any affect would have shown up by now.
- 19 comments
-
- connection
- gluten
-
(and 3 more)
Tagged with:
-
Blood sugar is the first thing I thought, too. Could be hyperglycaemia if the body cannot control blood sugar well. What happens if you eat a low carbohydrate, low glycaemic index meal?
-
Fuelling exercise -corn and other gluten free grains
Russ H replied to Gilly M's topic in Food Intolerance & Leaky Gut
Typical consumption of oxalate is approximately 1/5 g per day. The body doesn't store it. It is a tiny amount and not enough to be visible in the stool. In some people it can cause kidney stones. The coeliac diet is restrict enough without unnecessarily going on a low oxalic acid diet. -
Suspected celiac, advice appreciated!
Russ H replied to reecey's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Yes, get back on gluten and postpone the test if necessary. -
Fuelling exercise -corn and other gluten free grains
Russ H replied to Gilly M's topic in Food Intolerance & Leaky Gut
I think that it is very unlikely that you are passing visible calcium oxalate crystals in your stool. It is passed in urine. The vast majority of people do not have a problem handling oxalic acid. 'Oxalate dumping' does not exist. -
Mayo Testing Updates
Russ H replied to Tall Holly's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Thanks for the update. It is very helpful to others experiencing similar symptoms. No more gluten challenges and get on the mend! -
Fuelling exercise -corn and other gluten free grains
Russ H replied to Gilly M's topic in Food Intolerance & Leaky Gut
Hi Gilly, It is curious that you are passing oxalate crystals. Do you know for a fact that you are passing them? Oxalic acid is not particularly toxic in itself, it is just that it combines with calcium to produce calcium oxalate, which can cause kidney stones. Risk factors are not drinking enough water, consuming a lot of oxalic acid containing food... -
rye bread with no wheat ingredients
Russ H replied to stonefly's topic in Gluten-Free Foods, Products, Shopping & Medications
https://www.greatbritishchefs.com/recipes/pure-rye-bread-recipe -
rye bread with no wheat ingredients
Russ H replied to stonefly's topic in Gluten-Free Foods, Products, Shopping & Medications
Rye is absolutely not safe for people with coeliac disease. It has about 1/3 of the gluten of wheat, which is still far too much. -
IMU-856 Shows Promise as a Potential Treatment for Celiac Disease
Russ H commented on Jefferson Adams's article in Diagnosis, Testing & Treatment
I don't doubt your symptoms or reaction to gluten. It would be nice to have blood work to narrow it down as there is a whole spectrum of gluten related disorders.- 19 comments
-
- celiac disease
- drug
-
(and 3 more)
Tagged with:
-
Question about child's results
Russ H replied to scowt1's topic in Parents, Friends and Loved Ones of Celiacs
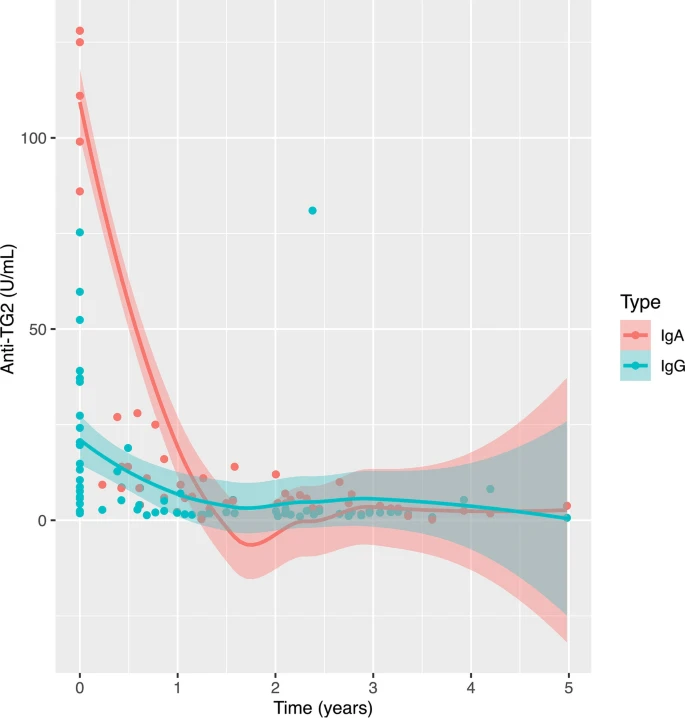
The common blood tests for coeliac disease look for antibodies to an enzyme found in the body called tissue transglutaminase 2 (tTG2) and to a fragment of gluten protein called deamidated gliadin peptide (DGP). EMA is endomysial antibody, which is basically a crude test for tTG2 - like running a tTG2 test with a high threshold so is less sensitive but more...