Russ H
Moderators-
Posts
446 -
Joined
-
Last visited
-
Days Won
8
Content Type
Profiles
Forums
Events
Blogs
Latest Celiac Disease News & Research:
Everything posted by Russ H
-
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
It is quite possible to have coeliac disease with negative or equivocal blood results. Make sure you keep eating gluten up to the endoscopy. In the UK, NICE recommends eating at least one gluten containing meal a day for 6 weeks prior to the endoscopy although they don't recommend how much gluten. -
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Do you have other symptoms? -
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
That paper does not measure isolated IgG DGP. Most of the positives for IgG DGP were also positive for IgA tTG, which you were not. Recent studies suggest that an isolated IgG DGP positive has poor predictive value (much less than 84%). Your test results neither confirm nor exclude coeliac disease. Here are some studies on isolated IgG DGP. Most... -
Which Fast Food French Fries are Gluten-Free?
Russ H commented on Jefferson Adams's article in Gluten-Free Foods & Beverages
That is a shame. In the UK, McDonalds fries are gluten-free.- 31 comments
-
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
An isolated IgG DGP has poor predictive power for coeliac disease. Below is a study that suggests somewhere around 82% of isolated IgG DGP positive tests are false positives. Due to the small study size though, there is a wide uncertainty in that figure, and up to 97.7% could be false positives. https://pubmed.ncbi.nlm.nih.gov/28161854/ -
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
OK, so basically the blood tests for coeliac disease look for antibodies to deamidated gliadin (which derives from gluten) and tissue transglutaminase (an enzyme that binds to gliadin in the gut). Two classes of antibodies are tested for (IgA and IgG), so this means 4 tests. Your tests show an isolated raised IgG deamidated gliadin antibody. Because of... -
Help understanding bloodwork
Russ H replied to Emma84's topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Hello and welcome to the forum. Do you have the reference ranges for those results? As they vary between labs, they are needed to interpret the results. -
It is likely the app. I don't use it as it is clunky and expensive for what it is. Whether or not an app said something was safe I always read the ingredients, which defeats the purpose. Food labelling in the UK is excellent, and clearly marks allergens. For finding places to eat, the 'Find Me Gluten Free' app is good.
-
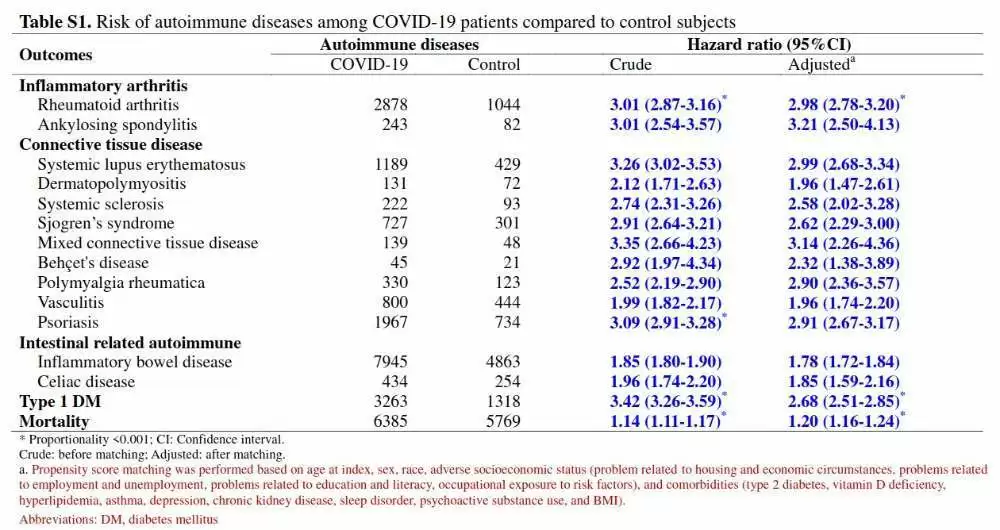
In Nature journal from earlier this year. In the unvaccinated, a COVID infection almost doubles the risk of developing coeliac disease. Further, in persons with a pre-existing autoimmune disease, COVID infection increases the risk of developing another autoimmune disease by 23%. The risk for vaccinated individuals was not investigated. Risk of autoimmune...
-
I have tried this recipe several times, and it is delicious - makes crispy batter. You have to be good to do it in 10 minutes though. I use self-raising gluten-free flour made by freee (contains rice flour, potato, tapioca, maize and buckwheat) and gluten-free beer for the batter. I also buy the tartar sauce ready made. https://www.youtube.com/watch...
-
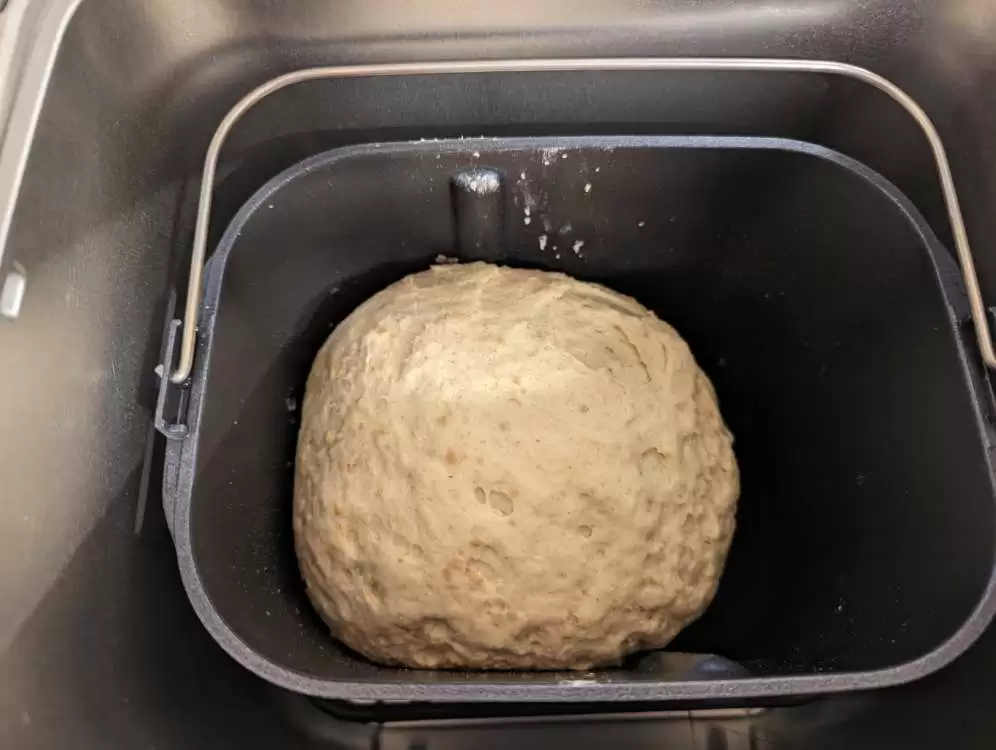
The gluten-free bread available in the UK is expensive and not very pleasant. I invested in a bread machine and tried the recipe linked below. It is a complicated recipe and I am going to try to simplify the ingredients. However, it works very well indeed and the resulting loaf smells and tastes like normal bread. This one is based on oat flour but there...
-
A good multivitamin and mineral tablet everyday for the first year. That said, the evidence points to gluten induced neuropathy being caused by a direct immunological attack rather than vitamin deficiency. Stick with a strict gluten-free diet. As your antibody levels fall, your symptoms should improve.
-
I think that you should concentrate on getting used to a strict gluten free diet and dealing with any nutritional deficiencies that you have (e.g. iron). That is difficult enough without disappearing down the rabbit hole of unproven pseudo-scientific diets.
-
This is false.
-
This won't help you. Coeliac disease is a serious condition, and you need to concentrate on reliable sources of information to help your recovery. This forum is full of knowledgeable people who can point you in the right direction.
-
Gluten is quite different to lectins, most of which are inactivated by cooking. Avoiding lectins would be very restrictive - avoiding gluten is difficult enough. Coeliac disease is a specific immune response to gluten. You can read about Steven Gundry and his pseudoscience here: https://sciencebasedmedicine.org/the-plant-paradox-steven-gundrys-war...
-
tTG2-IgA 10x or greater the standard upper limit is pretty sure to be coeliac disease. More moderate levels outside the standard range (as yours is) can be caused by coeliac disease but also other conditions such as Crohn's disease and rheumatoid arthritis. The EMA test is an old test that is relatively insensitive and course in its results due to the way...
-
Hello Mary Jean and welcome to the forum. I'm sorry you are struggling with the condition. It gets a lot easier as you learn what to eat and adapt your habits. As your gut heals you will also begin to feel much better. It can take up to 2 years to completely heal but most people improve much more quickly than this. I had terrible gas and it took 3 months...
-
Everything Worse After Celiac
Russ H replied to PrinceTrent's topic in Post Diagnosis, Recovery & Treatment of Celiac Disease
One of the symptoms I experienced was bloating, burping and reflux. That suddenly resolved after 3 months on a gluten free diet. Other symptoms gradually resolved over a year or so. -
Just getting started...
Russ H replied to a topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
That looks like a strong positive for anti-DGP antibodies. It is also possible to have antibodies against related enzymes tTG3 and tTG6 rather than the tTG2 that you were tested for. tTG3 is implicated in DH, and tTG6 in gluten induced neuropathy (GIN). Few centres test for these specific antibodies at the moment. It is also possible to have DH or GIN without... -
Just getting started...
Russ H replied to a topic in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Do you have the levels measured and standard ranges for those tests? I.e. are they borderline raised or very high? In young children, anti-DGP antibodies come up before anti-tTG but don't know if this is true in adults.